2552
Evaluating a Community-Based Diet and Lifestyle Intervention For Improved Metabolic Health in India: A Pilot Randomized Controlled Trial (RCT)1NIHR Nottingham Biomedical Research Centre, University of Nottingham, Nottingham University Hospitals NHS Trust and the University of Nottingham, Nottingham, United Kingdom, 2Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 3Metro Scan and Laboratory, Trivandrum, India, 4Population Health and Research Institute, Trivandrum, India, 5Centre for Research in the Behavioural Sciences, Nottingham University Business School, Nottingham, United Kingdom
Synopsis
The Indian population provides important cohorts for research into metabolic disorders due to the greater prevalence of NAFLD and diabetes, and the relatively low complexity of dietary intake. In this study 71 male participants with NAFLD were recruited from a cohort in India and randomized into two groups - a 16 week low glycaemic index dietary intervention arm and a control arm. 1H MRS was used to assess liver fat fractions, alongside other metabolic markers. Results show a trend towards reduced fat fractions in the diet arm only.
INTRODUCTION
South Asians are at higher risk of developing non-alcoholic fatty liver disease (NAFLD), diabetes and consequent mortality at a lower BMI than Caucasians [1]. This is due to a combination of genetic and lifestyle factors that lead to an increased susceptibility to metabolic syndrome. Previous studies have shown that lowering dietary Glycaemic Index (GI) in short term well controlled interventions improves glucose response [2] and reduces liver fat in energy matched diets [3]. This suggests that lowering GI could be a potentially beneficial lifestyle intervention to improve liver health, and would be particularly valuable in situations where high GI carbohydrate foods, such as white rice, make up the majority of energy intake in the diet (as is the case in many South Asian Countries).1H MRS provides a well validated, non-invasive technique to measure liver fat and can be used to monitor the effects of dietary interventions effectively [3, 4]. In this study, funded by Global Challenges Research Fund (GCRF), the effectiveness of lowering GI over a longer period whilst introducing regular Yoga sessions was evaluated in a community based intervention study in Kerala, South India.
METHODS
82 Men (18-70y) who consumed ≥5.7g/day.kg body weight of white rice were recruited from an established NAFLD cohort in Kerala, India and randomized to YOGA or YOGA+DIET arm. Both groups were offered sessions of 1hr up to 5 times/ week for 16 weeks. The YOGA+DIET group also replaced white rice consumption with a non-polished rice with low GI (Palakkadan matta). Protein intake was also increased by providing Mung Beans (2g protein per 100g rice vs 7g protein per 100g mung beans) which both lowered GI and in addition lowered glycaemic load (GL = GI x carbohydrate consumed). Blood samples, Oral Glucose Tolerance Test (OGTT) and MR scans were taken from patients at baseline and week 16, and pre v post values assessed using a two way ANOVA (data is shown as median and interquartile range).Blood samples were taken at the Kerala Public Health Research Institute (PHRI) and used to measure Insulin resistance (HOMA-IR), average blood glucose levels (HbA1c), Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST); postprandial blood glucose response was measured using OGTT.
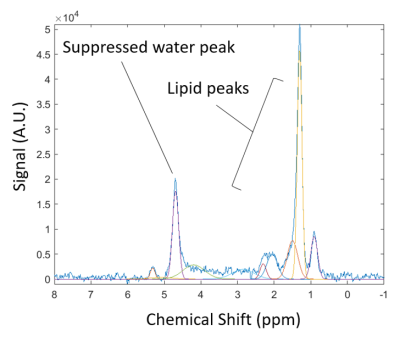
STEAM localized TE varying 1H MRS were acquired using a GE Signa Pioneer 3T scanner at the Metro Scan facility, Kerala. Spectra were acquired from a 20x20x20mm voxel in the right lower lobe of the liver over 4 breath-holds at varying echo times (TE=15, 60, 80 and 120 ms, TR = 3500, 4 averages per spectra) and an extra water suppressed spectra acquired at TE = 15. Spectra were post processed using in-house software providing automatic phase correction and frequency alignment before peak fitting using prior knowledge and tolerances [5]. Signal amplitudes of the water and lipid peaks at varying echo times were fitted to a mono-exponential T2 decay curve to determine water and lipid T2, and used to determine PDFF as described previously [6]
RESULTS
71 men (44.7 ± 10.8 y) completed the study. Groups were matched at baseline for age, BMI, HOMA-IR, HbA1c, ALT and AST.BMI, HbA1c, ALT and AST reduced significantly after both the 16 week YOGA and YOGA+DIET interventions, whilst fasting blood glucose was significantly lowered in the test arm ONLY (table 1).
Due to technical difficulties 1H MRS could not be assessed in 5 participants leaving 32 and 34 participants in the YOGA and YOGA+DIET groups respectively. MR Spectra had good SNR and were well resolved for individual peak fitting (figure 1). Baseline PDFF values in the YOGA and YOGA+DIET groups were 18.8 [14.8 – 21.6] % and 19.7 [16.3 – 25.1] % respectively and values in both groups reduced after the intervention (YOGA = 16.8 [13.9 – 21.6] %; YOGA+DIET = 18.6 [15.0 – 24.6] %) with reductions close to significance in the YOGA+DIET arm only (p = 0.07). There was a significant main effect of visit on PDDF values (p=0.004) but no significant interaction between visit and diet for any measured outcome.
DISCUSSION
The Indian population provides an important cohort for research into metabolic disorders due to the greater prevalence of NAFLD and diabetes, and the relatively low variability of dietary intake. Whilst multiple studies shave explored the short term effects of differing components of diet in a controlled environment, fewer studies have looked at the longer term effects of targeted ad libutum interventions. Participation in this study did produce improvements in metabolic health for all subjects. There was a trend for the dietary intervention to result in lower liver fat although this was not significant. Future studies should consider longer interventions or larger groups to increase statistical power.One of the main goals of GCRF is to support cutting-edge research that addresses the challenges faced by developing countries. During this study, new techniques were acquired and software written to further this development in India and increase research capacity.
Acknowledgements
No acknowledgement found.References
1. (NICE), N.I.f.H.a.C.E., BMI: Preventing Ill Health and Premature Death in Black, Asian and Other Minority Ethnic Groups. https://www.nice.org.uk/guidance/ph46/chapter/1-Recommendations, 2013.
2. Morgan, L.M., et al., Effect of meal timing and glycaemic index on glucose control and insulin secretion in healthy volunteers. British Journal of Nutrition, 2012. 108(7): p. 1286-1291. 3. Bawden, S., et al., Increased liver fat and glycogen stores following high compared with low glycaemic index food: a randomized cross over study. Diabetes Obes Metab, 2016.
4. Szczepaniak, L.S., et al., Measurement of intracellular triglyceride stores by H-1 spectroscopy: validation in vivo. American Journal of Physiology-Endocrinology and Metabolism, 1999. 276(5): p. E977-E989.
5. Hamilton, G., et al., In vivo characterization of the liver fat H-1 MR spectrum. Nmr in Biomedicine, 2011. 24(7): p. 784-790.
6. Stephenson, M.C., et al., Variability in fasting lipid and glycogen contents in hepatic and skeletal muscle tissue in subjects with and without type 2 diabetes: a 1H and 13C MRS study. NMR in Biomedicine, 2013. 26: p. 1518 - 1526.
Figures