2547
Comparison of breath-hold and respiratory-triggered 3D-SPACE MRCP sequences in the diagnosis of choledocholithiasis1XI’AN DAXING HOSPITAL, ShaanXi, Xi’an, China, 2Siemens Healthcare Ltd, ShaanXi, Xi’an, China
Synopsis
Magnetic resonance cholangiopancreatography (MRCP) is an effective imaging modality for the evaluation of anatomy and abnormalities of biliary and pancreatic system. The main drawback of conventional navigator-triggered (NT) MRCP is the long acquisition time resulting in a greater variability in the depth of respiration, which may create image blurring and motion artifacts. In this study, we performed MRCP scanning using a single breath hold (BH) 3D SPACE and NT SPACE protocols to evaluated the image quality and acquisition time in patients with choledocholithiasis.
Introduction
Magnetic resonance cholangiopancreatography (MRCP) is a standard imaging technique that provides detailed information of the pancreaticobiliary anatomy and pathology. Most initial study focused on 2D MRCP technique using breath-hold (BH) acquisition sequences, while they suffered from decreased spatial resolution and acquired non-isotropic voxel datasets. Therefore, for the purpose of obtaining high-resolution isotropic images, 3D navigator-triggered with Application-optimized Contrasts by using different flip angle Evolutions (NT-3D-SPACE) MRCP sequences have been performed principally with a respiratory-triggered technique during the last 10 years1. However, there is a clinical burden that the acquisition time of the respiratory-triggered 3D MRCP sequence often need take more than 6 minutes despite the use of parallel acquisition technique2. Breath-hold 3D SPACE(BH-3D-SPACE) is modified from product NT-3D-SPACE which need just about 18 seconds for breath-hold and have good image quality. The aim of this study was to compare the MRCP image quality between BH-3D-SPACE and NT 3D-SPACE, and furthermore to evaluate the diagnosis of choledocholithiasis in a routine clinical setting.Methods
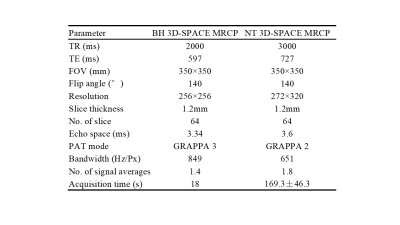
Seventy-eight patients (41 males and 37 females, age range 24-76 years) were enrolled in this study. All the patients underwent conventional NT-3D-SPACE and BH-3D-SPACE sequence on a 1.5T MR scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) using 6-channel body coil and 24-channel spine coil. The parameters about two different types of SPCAE sequences were as bellow: NT-3D-SPACE and BH-3D-SPACE. Two radiologists with five years of experience in abdominal radiology assessed the images independently. They evaluated the image quality of predefined segments of the pancreaticobiliary tree using a 5-point scale:1 = not displayed; 2 = incompletely displayed, not diagnostic;3 = all parts of the segments are uncertainly definable, still diagnostic; 4 = all parts of the segments are included, some are uncertainly definable, still diagnostic; 5 = all parts of the segments are completely and reliably definable. In a second step, the diagnostic confidence was rated on a 5-point scale from –2 to 2: –2 = reliably no concrement; –1 = most likely no concrement; 0 = not evaluable; 1 = most likely concrement; 2 = reliably recognized concrement. Evaluation of image quality and diagnostic confidence was done on the pancreaticobiliary tree which was subdivided into 9 segments. They were scored and statistically evaluated separately for visibility and diagnostic certainty by two blinded radiologists with differing levels of experience on a five-point scale of 1 to 5 and -2 to 2, respectively. Student t-test was performed, and the interobserver agreement was also calculated. Interobserver agreement was assessed by calculating the Cohen kappa statistic (kappa< 0.00: poor agreement, kappa = 0.00-0.20: slight agreement, kappa = 0.21-0.40: fair agreement, kappa = 0.40-0.60: moderate agreement, kappa = 0.61-0.80: substantial agreement; kappa = 0.81-1.00: almost complete agreement).Results
The mean acquisition time of BH-3D-SPACE MRCP was significantly shorter than that of NT-3D-SPACE MRCP (18 seconds vs 169.3±46.3 seconds; p< 0.001, Table 1). Image quality for each segment was significantly better for the BH-3D-SPACE sequence compared to the NT-3D-SPACE sequence (average score: BH 3D-SPACE 4.48±0.94 vs. NT-3D-SPACE 3.98±1.20, p< 0.01). Diagnostic confidence for the reporting radiologist was also significantly better for BH 3D-SPACE than for NT-3D-SPACE (average score: BH-3D-SPACE 1.67±0.53 vs. NT-3D-SPACE 1.41±0.67, p< 0.01). The interobserver agreement was high in both sequences, 0.68-0.91 and 0.61-0.83, respectively.Discussion and Conclusion
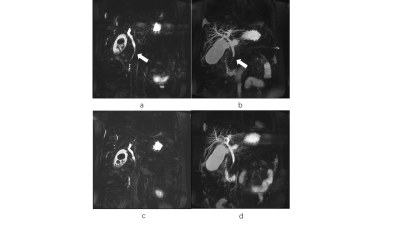
The study discovered that the BH-3D-SPACE sequence allows for better image quality and shorter data acquisition time in 1.5 T MRCP examinations and leads to a higher diagnostic confidence for choledocholithiasis compared to conventional NT-3D-SPACE sequence. It is known that navigator-triggered 3D-MRCP sequence have been widely used in clinical practice3. However, in patients with irregular or shallow respiratory rhythms, respiratory-gated acquisitions may fail to trigger correctly, prolonging scan times, or may result in images with substantial motion artifact. Our study confirmed that optimized BH-3D-SPACE MRCP is superior to conventional NT-3D-SPACE MRCP regarding the image quality and the level of diagnostic confidence for choledocholithiasis (Fig. 1). Because of the significantly better imaging results, we recommend replacing the conventional NT-3D-SPACE sequence with a BH-3D-SPACE protocol for patients with good BH capacity in 1.5 T MRCP examinations.Acknowledgements
We thank Shaoyu Wang of Siemens Healthcare, Ltd., Xi’an, China, for technical support.References
1.Zins M. Breath-holding 3D MRCP: the time is now? European Radiology 2018; 28(9): 3719-3720.
2 .Sudholt P, Zaehringer C, Urigo C, Tyndall A, Bongartz G, Hohmann J. Comparison of Optimized 3D-SPACE and 3D-TSE Sequences at 1.5T MRCP in the Diagnosis of Choledocholithiasis. Rofo 2015; 187(6): 467-471.
3.Taron J, Weiss J, Notohamiprodjo M, et al. Acceleration of Magnetic Resonance Cholangiopancreatography Using Compressed Sensing at 1.5 and 3 T: A Clinical Feasibility Study. Investigative Radiology 2018; 53: 1.
Figures