2545
Pancreaticobiliary System Evaluation via BH-MRCP using SPACE: A Comparison with Conventional NT-MRCP at 3 Tesla1The Third Affiliated Hospital,Sun Yat-sen University, Guangzhou, China, 2MR Collaborations, Siemens Healthcare Ltd, Shenzhen, China, 3Siemens Healthcare Ltd, Guangzhou, China
Synopsis
Conventional three-dimensional navigator-triggered magnetic resonance cholangiopancreatography (NT-MRCP) is widely used in clinics for the evaluation of the anatomy and abnormalities of the pancreaticobiliary system. However, the method has limitations because of its extensive time to acquire images. This study explored the efficiency and the clinical utility of 3D breath-hold MRCP (BH-MRCP) as an alternative to conventional NT-MRCP at 3 Tesla. Based on these, methods used on a sample population of 25 patients, the results showed that the BH-MRCP technique can be a viable alternative to enhance the clinical workflow of pancreatobiliary MRI.
Introduction
Conventional three-dimensional (3-D) navigator-triggered magnetic resonance cholangiopancreatography (NT-MRCP), based on the sampling perfection with application-optimized contrasts using different flip-angle evolutions (SPACE) sequence, is widely used as a noninvasive imaging technique to evaluate the anatomy and any abnormalities of the pancreaticobiliary system [1]. However, the main drawback of this approach is its long acquisition time, which can render variability in the respiration depth. Consequently, images are prone to blurred effects and motion artifacts [2]. Therefore, this study aimed to investigate the clinical utility of 3D single-breath-hold SPACE MRCP (BH-MRCP) with multi-channel receiver coils and to compare it with conventional NT-MRCP on a 3-Tesla magnetic resonance (3T MR) scanner.Methods
Between September 2019 and October 2019, 25 patients (12 male and 13 female; age range, 33-60 years) who were determined by clinical evaluation to have suspected pancreaticobiliary diseases were enrolled in the study. The IRB-approved MR examinations were performed on a 3T MR scanner (Magnetom Prisma, Siemens Healthcare, Erlangen, Germany) using an 18-channel body matrix coil combined with a 32-channel spine matrix coil. Free-breathing 3D NT-MRCP and single-BH 3D MRCP in a single-oblique coronal orientation were performed on each patient without contrast material. The imaging parameters of the BH-MRCP sequence were as follows: FOV= 340 x 340 mm2, TR/TE=2000/606ms, slice thickness=1.3mm, imaging matrix=320x224, acquired voxel size=0.5x0.5x1.3mm3, bandwidth = 822Hz/Px, acquisition time (TA)=18s. echo-train length=380, acceleration factor of GRAPPA=4. In comparison, the imaging parameters of NT-MRCP were: FOV= 340x340 mm2, TR/TE=1800/574ms, slice thickness=1.1mm, imaging matrix=320x224, acquired voxel size=0.5x0.5x1.1mm3, bandwidth = 822Hz/Px,. echo-train length=240, acceleration factor of GRAPPA=3, the TA for all the enrolled subjects =208±47s.Rotating maximum-intensity-projection (MIP) images of both sequences were used for the image display. Subjective image quality was independently scored by two radiologists with experience reading abdominal MRI examinations using a 4-point rating scale from lowest to highest (1 = poor, 4 = excellent) on the assessment of hepatic segmental bile duct, right and left hepatic duct, common bile duct, gallbladder, pancreatic duct, and overall image quality on MIP images, For quantitative objective assessment, the contrast-to-noise ratio (CNR) between the common bile duct(CBD) and their surrounding tissues was calculated and compared between the two techniques. The image scores and the quantitative parameters were compared using the Wilcoxon signed-rank test. A P value having less than 0.05 was considered significant.
Results
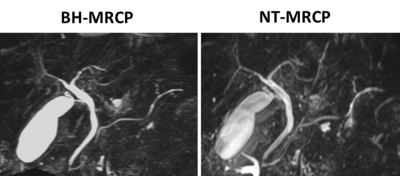
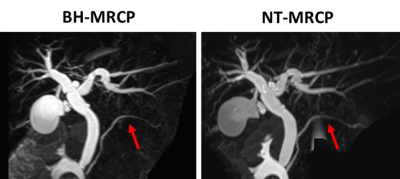
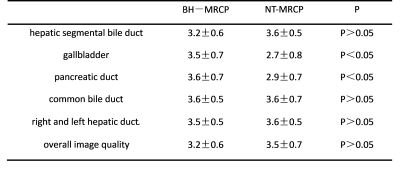
Among the 25 patients, 5 of them were respiratory disordered. The MIP images that were acquired on these patients using NT-MRCP showed blurring artifacts larger than those seen on MIP images acquired using BH–MRCP (Figure 1). The remaining 20 patients underwent MRCP and were categorized as having the following conditions: hepatic segmental bile duct stones (n=3), gallbladder stones (n=5), common bile duct stones (n=3), ampullary carcinoma (n=2), cholecystitis (n=3), pancreatic carcinoma (n=1), and none (ie, normal patients, n=3). No significant difference was found between the two sequences for the diagnosis of the patients (p>0.05). As Table 1 and Figure 2 show, the image scores of the BH-MRCP sequence were higher than those of the NT-MRCP sequence in the gallbladder, (3.5±0.7 vs. 2.7±0.8, p<0.05); and the pancreatic duct (3.6±0.7 vs. 2.9±0.7 p < 0.05). In a comparison of the image scores between the two sequences, there was no significant difference found in hepatic segmental bile duct (3.2±0.6 vs. 3.6±0.5, p>0.05), common bile duct (3.6±0.5 vs. 3.6±0.7, p>0.05), right and left hepatic duct 3.5±0.53 vs. 3.6±0.52, p>0.05). Overall image quality was not found significantly different between the two sequences (3.2±0.6 vs. 3.5±0.7, p>0.05). The mean CNR of BH-MRCP (7.3±2.4 ) was slightly lower than that of NT-MRCP (10.4±3.7, p < 0.05).Discussion and Conclusion
In this work, we investigated the utility of 3D SPACE BH-MRCP and compared the method with conventional NT-MRCP in clinics. We found that for patients suffering from respiratory disorder, the BH-MRCP yields an improved perceived image quality in a single breath-hold (18 seconds) compared to conventional NT-MRCP. For patients without respiratory disorder, the BH-MRCP yields similar diagnostic performance with NT-MRCP. The findings suggest that the BH-MRCP technique may be a viable alternative to the conventional method, which can enhance the clinical workflow of pancreatobiliary MRI.Acknowledgements
References
1. Morita S, Ueno E, Suzuki K, et al. Navigator-triggered prospective acquisition correction (PACE) technique vs. conventional respiratory-triggered technique for free-breathing 3D MRCP: an initial prospective comparative study using healthy volunteers. J Magn Reson Imaging 2008; 28:673–677.
2. Chen Z, Sun B, Duan Q, et al. Three-Dimensional Breath-Hold MRCP Using SPACE Pulse Sequence at 3 T: Comparison With Conventional Navigator-Triggered Technique[J]. American Journal of Roentgenology, 2019: 1-6.
Figures