2544
Clinical feasibility of compressed SENSE accelerated MRCP with Vital Eye in pancreaticobiliary disorders: a preliminary study.1Department of radiology, Peking Union Medical College Hospital, Beijing, China, 2Philips Healthcare, Beijing, China
Synopsis
The purposes of this study were to prospectively evaluate the clinical feasibility of a MRCP protocol using both Vital Eye and compressed SENSE(CS-VE-MRCP) and to compare its performance with original navigator-triggered (NT) CS-NT-MRCP and NT-MRCP. The results show that the imaging quality and diagnostic performance of CS-VE-MRCP was comparable to that of NT-MRCP and slightly superior than that of CS-NT-MRCP. Besides, the scan time of CS-VE-MRCP was significantly decreased compared to that of NT-MRCP. The combination of compressed SENSE and Vital Eye in MRCP was feasible, suggesting the potential of imaging time reduction without pampering the diagnostic capability.
Recently, a real-time tracking (Vital Eye) technique, a revolution in patient sensing using adaptive intelligence to detect even the tiniest microscopic signs of breathing was developed. The quality of the physiology signal is better than a belt-based approach based upon faster, more accurate, detection of breathing. With Vital Eye, the technologist no longer needs to set up an old-fashioned respiratory belt as well as breath training, but receives a continuous and robust respiratory signal without any interaction. It allows routine exam set-up time to occur in less than a minute, even for less experienced operators. But the clinical feasibility need to be investigated.
So, the purposes of this study were to prospectively evaluate the clinical feasibility of a MRCP protocol using both Vital Eye and compressed SENSE(CS-VE-MRCP) and to compare its performance with original navigator-triggered (NT) CS-NT-MRCP and NT-MRCP.
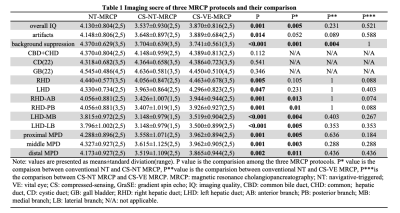
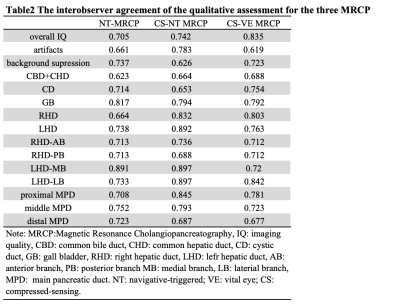
Materials and methods:A total of 35 patients (18 males, 17 females, age range:15-60 years, mean age: 45.67±16.72 years) suspected pancreaticobiliary pathologies were prospectively enrolled and done the three MRCP protocol randomly. The acquisition time was recorded. The imaging assessment was based on a 5-point scale by 2 radiologists independently, which included the following four parts: overall imaging quality, background suppression, artifacts, and the duct visualization. For duct visualization, the entire pancreaticobiliary system was divided into the 12 segments: the common bile and hepatic ducts as an integral segment (CBD+CHD), the cystic duct (CD), the gallbladder (GB), the right hepatic duct (RHD), the anterior branch of the right hepatic duct (RHD-AB), the posterior branch of the right hepatic duct (RHD-PB), the left hepatic duct (LHD), the medial branch of the left hepatic duct (LHD-MB), the lateral branch of the left hepatic duct (LHD-LB), and the proximal / middle / distal parts of the main pancreatic duct (P-MPD, M-MPD, and D-MPD respectively). The Friedman test with a post hoc test was performed to compare image acquisition time, the presence of artifacts, background suppression, overall image quality, and duct visualization among the three protocols. The diagnosis performance of the three protocols were evaluated by the AUC value and compared by Delong’s test. The inter-observer agreement was evaluated by linearly weighted kappa coefficients.
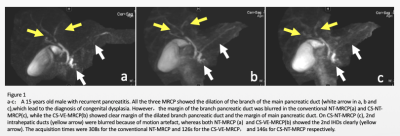
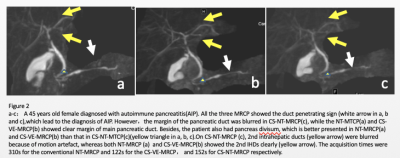
Results: The acquisition time was 135-172, 148-183, and 283-325 seconds for CS-VE-MRCP, CS-NT-MRCP and NT-MRCP, respectively. Compared to NT-MRCP, the acquisition time of CS-NT-MRCP and CS-VE-MRCP was significantly decreased (both P < 0.001). There is no significant difference in overall imaging quality(P﹥0.05) between the NT-MRCP and CS-VE-MRCP protocols. CS-VE-MRCP depicted pancreatic duct and intrahepatic duct better than CS-NT-MRCP (all P < 0.05) and comparable with NT-MRCP (all P﹥0.05)(Table 1). For detecting pancreatobiliary pathologies, both CS-VE-MRCP and NT-MRCP had significantly better performance compared to CS-NT-MRCP (AUC was 0.955(95%CI:0.918,1) for NT-MRCP, 0.903(95%CI:0.839, 0.968) for CS-VE-MRCP and 0.677(95%CI:0.573,0.781) for CS-NT-MRCP, both P < 0.05) (Figure 1 and Figure 2). All evaluation reached good to excellent agreement (0.619-0.897) (Table 2).
Discussion: This preliminary study shows that the imaging quality and diagnostic performance of CS-VE-MRCP was comparable to that of NT-MRCP and slightly superior than that of CS-NT-MRCP. Besides, the scan time of CS-VE-MRCP was significantly decreased compared to that of NT-MRCP. The combination of compressed SENSEN and Vital Eye in MRCP was feasible, suggesting the potential of imaging time reduction without pampering the diagnostic capability. Besides, using Vital Eye is expected to useful in improving and predigesting the workflow by omitting the process of setting up an old-fashioned respiratory belt as well as breath training, especially for technologists with less experience.
Conclusions: CS-VE-MRCP is feasible in patients suspected with pancreaticobiliary diseases.
Acknowledgements
N/AReferences
1. Zaitsev M, Maclaren J, Herbst M. Motion artifacts in MRI: A complex problem with many partial solutions. Journal of magnetic resonance imaging : JMRI 2015;42(4):887-901.
2. Anupindi SA, Victoria T. Magnetic resonance cholangiopancreatography: techniques and applications. Magn Reson Imaging Clin N Am 2008;16(3):453-466, v.
3. He M, Xu J, Sun Z, et al. Comparison and evaluation of the efficacy of compressed SENSE (CS) and gradient- and spin-echo (GRASE) in breath-hold (BH) magnetic resonance cholangiopancreatography (MRCP). Journal of magnetic resonance imaging : JMRI 2019.
4. Zhu L, Wu X, Sun Z, et al. Compressed-Sensing Accelerated 3-Dimensional Magnetic Resonance Cholangiopancreatography: Application in Suspected Pancreatic Diseases. Invest Radiol 2018;53(3):150-157.
5. Yoon JH, Lee SM, Kang HJ, et al. Clinical Feasibility of 3-Dimensional Magnetic Resonance Cholangiopancreatography Using Compressed Sensing: Comparison of Image Quality and Diagnostic Performance. Invest Radiol 2017;52(10):612-619.
6. Zhang J, Israel GM, Hecht EM, Krinsky GA, Babb JS, Lee VS. Isotropic 3D T2-weighted MR cholangiopancreatography with parallel imaging: feasibility study. AJR Am J Roentgenol 2006;187(6):1564-1570.
7. Zhu L, Sun ZY, Xue HD, et al. Patient-adapted respiratory training: Effect on navigator-triggered 3D MRCP in painful pancreatobiliary disorders. Magnetic resonance imaging 2018;45:43-50.
Figures