2534
Diagnostic accuracy of bladder invasion in cervical cancer: Comparison of T2-weighted, diffusion-weighted, and contrast-enhanced MR imaging.1Department of Medical Imaging and Intervention, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan, 2Imaging Core Laboratory, Institute for Radiological Research, Chang Gung Memorial Hospital at Linkou and Chang Gung University, Taoyuan, Taiwan, 3Department of Diagnostic Radiology, Chang Gung Memorial Hospital at Keelung, Keelung, Taiwan, 4Clinical Metabolomics Core Laboratory, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
Synopsis
Cervical cancer with bladder invasion is rare and carries a poor prognosis. MR imaging is useful in the detection of bladder mucosal involvement from cervical cancer, with reported high negative predictive value, and therefore can serve to justify the necessities of invasive cystoscopy. Diffusion-weighted imaging is superior to T2-weighted and contrast-enhanced MR study in accurately diagnosing bladder invasion.
Introduction
Locally advanced cervical cancer with bladder invasion is rare, represents only 2% of cervical cancers, and carries a poor prognosis, with an estimated 5-year overall survival of 20% 1. Standard diagnosis relies on cystoscopy and biopsy. Pre-treatment pelvic MR study has a high reported staging accuracy and negative predictive value for ruling out bladder invasion, and there can be used to guide the necessities of invasive cystoscopy 2,3. We aim to investigate the diagnostic accuracy of magnetic resonance (MR) sequences in diagnosing bladder invasion in cervical cancer patients.Methods
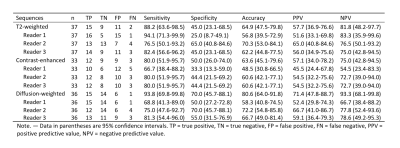
Our institutional review board approved this Health Insurance Portability and Accountability Act-compliant retrospective study. From a review of our pathology database records between January 2010 and December 2017, we identified 37 cases with pathological proven cervical cancer who also received cystoscopy and biopsy during the time of diagnosis. Three radiologists with 1, 5, 9 years of experience in gynecologic radiology independently evaluated imaging features in T2-weighted, diffusion-weighted (DW), apparent diffusion coefficient (ADC) mapping, and contrast-enhanced (CE) MR images. The sensitivity, specificity, and diagnostic accuracy of imaging features were studied. Reader agreement on imaging features and interobserver variability were analyzed using weighted kappa statistics.Results
In our cohort, 17 patients out of 37 had bladder invasion from cervical tumors. DW imaging had the best performance in the evaluation of bladder mucosa invasion, with an accuracy of 80.6%, sensitivity of 93.8% and specificity of 70.0%, comparing to CE MR (63.6%, 80.0%, and 50%) and T2-weighted MR (65.9%, 88.2%, and 45.0%). Altogether, the MR study yielded a 100% negative predictive value (NPV). Reader’s agreement is good in CE MR (k = 0.8), moderate in DW imaging (k = 0.45) and poor in T2-weighted imaging (k = 0.33).Conclusion
Diffusion-weighted imaging is superior to T2-weighted and contrast-enhanced MR study in the detection of bladder mucosal involvement from cervical cancer.Acknowledgements
The authors acknowledge the assistance provided by the Cancer Center of Chang Gung Memorial Hospital, Linkou, Taiwan. Supported by Chang Gung Medical Foundation grant CIRPG3H0011.
References
1. Sun R, Koubaa I, Limkin EJ, et al. Locally advanced cervical cancer with bladder invasion: clinical outcomes and predictive factors for vesicovaginal fistulae. Oncotarget. 2018;9(10): 9299-9310.
2. Rockall AG, Ghosh S, Alexander-Sefre F, et al. Can MRI rule out bladder and rectal invasion in cervical cancer to help select patients for limited EUA? Gynecol Oncol. 2006;101(2):244-249.
3. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Cervical Cancer (Version 5.2019). https://www.nccn.org/professionals/physician_gls/PDF/cervical.pdf. Accessed 5 Nov 2019.
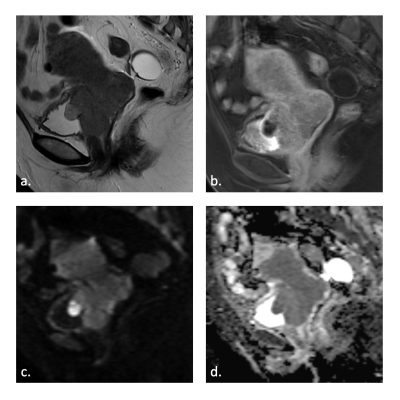
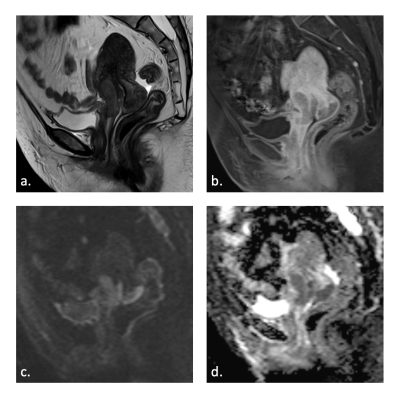
Figures