2531
Development of fetal MRI in a tertiary referral center: how it impacts prenatal diagnosis and alters clinical outcome
Jonan Chun Yin Lee1, Renata Kiri Mak1, and Janice Wong Li Yu1
1Radiology, Queen Elizabeth Hospital, Hong Kong, Hong Kong
1Radiology, Queen Elizabeth Hospital, Hong Kong, Hong Kong
Synopsis
Fetal MRI is a useful investigation to visualize congenital anomalies and allow for appropriate counselling and timely intervention. Since early 2017, our hospital has begun to perform fetal MRI from obstetric referrals. 18 pregnant patients underwent fetal MRI for suspected fetal anomalies. The neurological system was the most common region of concern during fetal MRI (67%). When compared to antenatal ultrasonography, fetal MRI provided significant additional and/or change in diagnostic information in 44% of patients , and results in change in postnatal outcome and/or facilitation of postnatal management in 44% of patients, including termination of pregnancy and prompt surgical intervention.
Introduction
Congenital anomalies are an important cause of fetal, neonatal and childhood morbidity and mortality. Currently, antenatal structural ultrasounds are commonly used for prenatal detection. However, ultrasound has limitations including operator-dependence and suboptimal soft tissue definition. Fetal MRI presents itself as a useful second-line investigation to visualize these anomalies. Since early 2017, our hospital has begun to perform fetal MRI from obstetric referrals. Here, we investigate the utility of MRI in aiding the diagnosis or congenital anomalies, and in affecting subsequent management.Methods
From March 2017 to Oct 2019 All pregnant patients with suspected fetal structural anomalies referred to the Department of Radiology & Imaging, Queen Elizabeth Hospital, Hong Kong for fetal MRI were retrospectively reviewed. Fetal MRI studies were cross-examined with antenatal structural ultrasound findings, obstetric and postnatal outcomes.Results
A total of 18 pregnant patients underwent fetal MRI for suspected fetal anomalies. This includes 16 singleton pregnancy and 2 twin pregnancies. Majority of them were performed in third trimester (14/18, 78%). The neurological system was the most common region of concern during fetal MRI, accounting for 12 out of 18 cases (67%), followed by cardiopulmonary and gastrointestinal systems (both 11%). When compared to antenatal ultrasonography, fetal MRI provided significant additional and/or change in diagnostic information in 44% of patients (8/18), and results in change in postnatal outcome and/or facilitation of postnatal management in 44% of patients (8/18), including termination of pregnancy, early prompt postnatal surgical intervention and early multidisciplinary input. No maternal or fetal adverse events associated with MRI have been reported in our study.Case illustrations
Three cases will be illustrated in further details to highlight the utility of fetal MRI in eastablishing the diagnosis and altering the pregnancy or postnatal outcome. They are:1) a case of acrocallosal syndrome with termination of pregnancy after fetal MRI.
2) a case of small bowel atresia with in-utero perforation and meconium pseudocyst with prompt drainage of cysts after birth and early surgical resection.
3) a case of fetal vascular insult with cystic encephalomalacia after co-twin demise in monochorionic pregnancy.
Conclusion
Fetal MRI either corrected the diagnosis or offered additional diagnostic information, altering the outcome for almost half of the cases reviewed. It is a powerful complement to structural ultrasound for the evaluation of a variety of fetal anomalies. There is potential in further expanding the field of fetal MRI, e.g. cardiac dynamic imaging etc.Acknowledgements
Dr KY Leung and Dr NY Yu, Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Hong KongReferences
Reference: (1) P.A. Boyd et al. Monitoring the Prenatal Detection of Structural Fetal Congenital Anomalies in England and Wales: A Register-based stydy. Journal of Medical Screening. May 2011; 18:2-7 (2) Manganaro et al. Highlights on MRI of the fetal body. La Radiologia Medica. April 2018; 123(4):271-285Figures
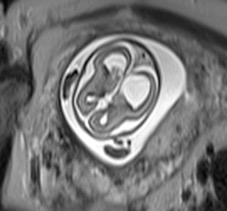
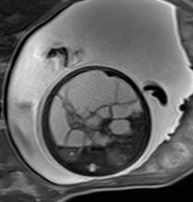
(1a) a
case of acrocallosal syndrome with termination of pregnancy after fetal MRI
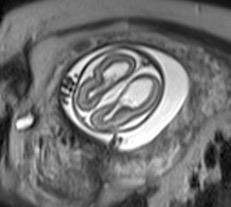
(1b) a
case of acrocallosal syndrome with termination of pregnancy after fetal MRI
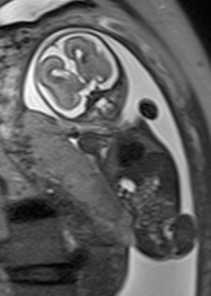
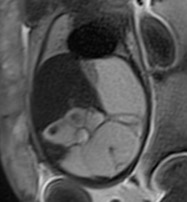
(1c) a
case of acrocallosal syndrome with termination of pregnancy after fetal MRI
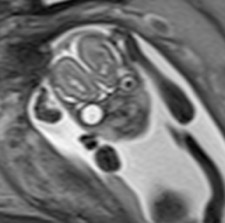
(1d) a
case of acrocallosal syndrome with termination of pregnancy after fetal MRI
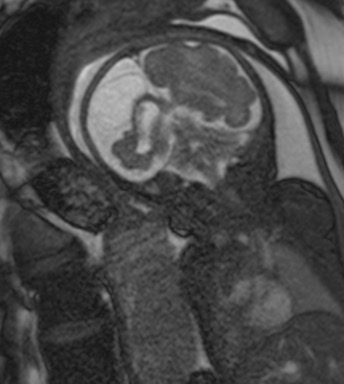
(2a) a
case of small bowel atresia with in-utero perforation and meconium pseudocyst
with prompt drainage of cysts after birth and early surgical resection.
(2b) a
case of small bowel atresia with in-utero perforation and meconium pseudocyst
with prompt drainage of cysts after birth and early surgical resection.

(2c) a
case of small bowel atresia with in-utero perforation and meconium pseudocyst
with prompt drainage of cysts after birth and early surgical resection.
(3a) a case of fetal vascular insult with cystic
encephalomalacia after co-twin demise in monochorionic pregnancy
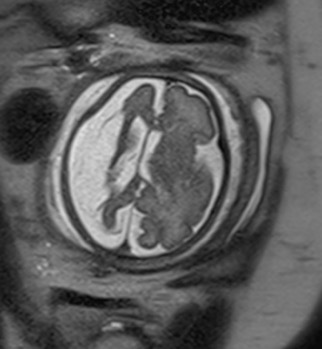
(3b) a case of fetal vascular insult with cystic
encephalomalacia after co-twin demise in monochorionic pregnancy