2508
Acute pancreatic fat change in probiotics and intermittent fasting trial1School of Science, Auckland University of Technology, Auckland, New Zealand, 2School of Medicine, University of Auckland, Auckland, New Zealand, 3Canterbury Health Laboratories, Canterbury District Health Board, Christchurch, New Zealand, 4Saint Kentigern College, Auckland, New Zealand
Synopsis
Pancreatic fat has been reported to be closely related to type 2 diabetes risk, hence is the subject of our investigation in a clinical trial. Pancreatic fat changes before and after a 12-week intermittent fasting programme with or without daily probiotic were determined using magnetic resonance imaging (MRI). Two-point Dixon protocol was used to scan patients and manual image-processing method was used to quantify the fat. A significant reduction in pancreatic fat was observed after intermittent fasting, while addition of probiotic did not increase pancreatic fat reduction.
Introduction
Accumulation of ectopic fat in the pancreas has been linked to type 2 diabetes risk 1,2,3. Probiotic supplementation has been reported to be effective in glycemic control 4. Intermittent fasting has been shown to have positive effect on the control and prevention of type 2 diabetes, improving several metabolic indices including body weight, fasting glucose and postprandial variability 5. However, the effect of those interventions on pancreatic fat, which is a key risk factor of type 2 diabetes, has not been thoroughly investigated. The most accurate ectopic fat measurement is via magnetic resonance (MR) technique6-9. In this study, we conducted a clinical trial to study the effect of intermittent fasting with or without a probiotic supplement on pancreatic fat, using MRI as a tool for pancreatic fat quantification. The objective of this project was to study pancreatic fat changes in relation to interventions.Methods
This is a parallel randomised, placebo-controlled trial to test the treatment effect of daily L rhamnosus HN001 (6x109 cfu)/placebo capsule with intermittent (5:2) fasting in New Zealand adults with prediabetes. Men and women aged over 18 years of age with prediabetes defined as HbA1c between 40-49mmol/mol and BMI > 35 were recruited. Exclusion criteria are known diabetes or pregnancy, medical conditions or medications likely to affect the assessment for diabetes. In total, 24 patients were recruited. Twelve each were assigned to the intermittent fasting with placebo group and the intermittent fasting with probiotic group. Patients followed the prescribed dietary programme for 12 weeks. They were MR-scanned before and after the dietary intervention. Each patient was scanned for the entire abdomen by a 3.0 Tesla Siemens MR scanner. A 3D dual gradient-echo sequence acquired water/fat images in one acquisition using a 2-point Dixon technique. T1-weighted spin echo pulse sequence was used with: TR, 6.5 msec, TE, 2.4/4.8 msec, flip angle, 12 degrees, matrix, 256 x 128, and 0.7 excitation. The pancreas was scanned using a similar protocol, with 12-second breath hold and a number of 5.0 mm slices were planned across the pancreas. For fat volume determination in pancreas, two methods were used. The first method used two independent operators to process the images manually in ImageJ. The coverage of the entire pancreas including slices and boundaries in water-only and water-fat images was determined, and volume calculated. Then, the fat volume within all above-determined pancreas slices was calculated in the fat-only images and the fat volume percentage of the entire pancreas was deduced. A second method was employed to validate the results of the first method which is termed MR-OPSY method 10. Three 100 mm2 regions of interest (ROIs) were selected in head, body and tail of one slice of pancreas image. Then the fat area against the ROI area was determined in the fat-only images, which represents the percentage of fat in the entire pancreas.Results
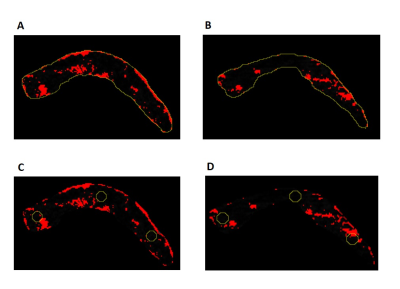
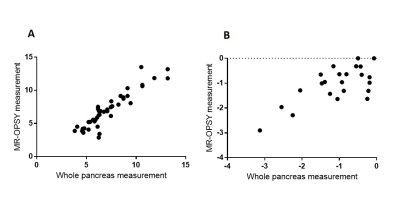
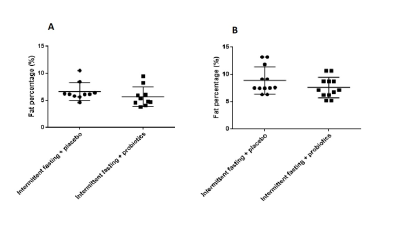
Ten patients completed MRI study in the intermittent fasting with placebo group and twelve patients completed MRI scans in the intermittent fasting with probiotic group. Figure 1 shows an example of fat determination in pancreas with two methods. Figure 2 shows significant Pearson’s correlation of the pancreatic fat percentage numbers (44 pairs of number) determined by two methods (r value 0.9235), as well as the resulting pancreatic fat change of the 22 patients calculated by two methods (r value 0.7016). Both intermittent fasting for 12 weeks with and without probiotics produced significant pancreatic fat reduction (p = 0.0009 and 0.0027, respectively, Figure 3). However, there is no significant difference of pancreatic fat loss between the two groups (p = 0.2269, Figure 4).Discussion
This is the first study to assess changes in pancreatic fat using MRI in prediabetes patients on intermittent fasting with probiotic or placebo supplement for 12 weeks. The two post-scan image processing method appears to correlate well in general, providing similar outcomes. The MROPSY method is easy to operate and involves less calculation. The whole pancreas analysis method is more labour intensive. However, the ROI selections in images from before and after intervention may not be near identical. This may introduce errors because of inhomogeneity of fat distribution in the pancreas, especially when sample size is small. Our study shows that intermittent fasting can reduce pancreatic fat significantly, which is a key risk factor of type 2 diabetes, in a relatively short period of time. The addition of probiotics, on the other hand, does not add any extra benefit in terms of pancreatic fat reduction.Conclusion
MRI method is a useful tool to measure pancreatic fat change in clinic, which may provide type 2 diabetes risk indication. Lifestyle change, such as intermittent fasting, can definitely reduce the type 2 diabetes risk in obese and prediabetic patients. Probiotics on the other hand, may not provide direct benefit to type 2 diabetes risk reduction, particularly in terms of pancreatic fat reduction.Acknowledgements
This research was supported by a grant from Health Research Council of New ZealandReferences
1. Heni M, Machann J, Staiger H, Schwenzer NF, Peter A, Schick F, et al. Pancreatic fat is negatively associated with insulin secretion in individuals with impaired fasting glucose and/or impaired glucose tolerance: a nuclear magnetic resonance study. Diabetes/metabolism research and reviews. 2010;26(3):200-5.
2. Toledo-Corral CM, Alderete TL, Hu HH, Nayak K, Esplana S, Liu T, et al. Ectopic fat deposition in prediabetic overweight and obese minority adolescents. The Journal of Clinical Endocrinology & Metabolism. 2013;98(3):1115-21.
3. Singh RG, Yoon HD, Wu LM, Lu J, Plank LD, Petrov MS. Ectopic fat accumulation in the pancreas and its clinical relevance: A systematic review, meta-analysis, and meta-regression. Metabolism-Clinical and Experimental. 2017;69:1-13.
4. Luoto R, Laitinen K, Nermes M, Isolauri E. Impact of maternal probiotic-supplemented dietary counselling on pregnancy outcome and prenatal and postnatal growth: a double-blind, placebo-controlled study. British journal of nutrition. 2010;103(12):1792-9.
5. Arnason TG, Bowen MW, Mansell KD. Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study. World Journal of Diabetes. 2017;8(4):154-64.
6. Kim H, Taksali SE, Dufour S, Befroy D, Goodman TR, Petersen KF, et al. Comparative MR study of hepatic fat quantification using single‐voxel proton spectroscopy, two‐point dixon and three‐point IDEAL. Magnetic Resonance in Medicine. 2008;59(3):521-7.
7. Springer F, Machann J, Claussen CD, Schick F, Schwenzer NF. Liver fat content determined by magnetic resonance imaging and spectroscopy. World journal of gastroenterology: WJG. 2010;16(13):1560.
8. Machann J, Thamer C, Schnoedt B, Haap M, Haring HU, Claussen CD, et al. Standardized assessment of whole body adipose tissue topography by MRI. Journal of Magnetic Resonance Imaging. 2005;21(4):455-62.
9. Hu HH, Kim HW, Nayak KS, Goran MI. Comparison of Fat–Water MRI and Single‐voxel MRS in the Assessment of Hepatic and Pancreatic Fat Fractions in Humans. Obesity. 2010;18(4):841-7.
10. Al-Mrabeh A, Hollingsworth KG, Steven S, Tiniakos D, Taylor R. Quantification of intrapancreatic fat in type 2 diabetes by MRI. PLoS One. 2017;12(4):e0174660.
Figures