2490
Prediction of post-hepatectomy liver function with Dynamic Gadoxetate-Enhanced MRI1University of Leeds, Leeds, United Kingdom, 2Department of Medical Physics, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom, 3Leeds Institute of Data Analytics, University of Leeds, Leeds, United Kingdom, 4Hepatobiliary and Transplantation Surgery, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom, 5Department of Radiology, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom, 6Department of Infection, Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom
Synopsis
The aim of this study was to identify Dynamic Gadoxetate-Enhanced MRI (DGE-MRI) biomarkers that can improve predictions of post-hepatectomy liver function. 29 patients requiring resection for colorectal liver metastases were recruited, with post-operative bilirubin as outcome measure. The results suggest that: (a) functional imaging substantially improves outcome predictions over demographical and biochemical tests; (b) it is critical to separately characterise the future liver remnant; (c) volumetry does not offer any added predictive value. We conclude that DGE-MRI may improve patient selection for hepatectomy, potentially reducing the risk of post-hepatectomy liver failure while allowing more patients to be operated.
INTRODUCTION
Major liver resection is the only curative option for many patients with primary or secondary liver cancer but is associated with a risk of post-hepatectomy liver failure (PHLF)1. A reliable preoperative estimate of post-operative liver function would help to reduce the risk of PHLF, optimise surgery planning and potentially open up this treatment option in cases where this is currently considered too risky. Hepatobiliary Scintigraphy has demonstrated that there is a role for imaging-based measurement of partial liver function2, but the technique is underused in clinical practice.Dynamic Gadoxetate-enhanced MRI (DGE-MRI) is a more widely available imaging method with potential to measure partial liver function3. Gadoxetate is filtered by hepatocytes through OATP1, MRP2 and MRP3 transporters, a mechanism shared with bilirubin excretion. Liver function of individual segments can be quantified by DGE-MRI and thus potentially provide a direct prediction of post-operative liver function.
The aim of this study was to determine which, if any, pre-operative DGE-MRI biomarkers of liver function have the potential to improve prediction of post-operative outcomes over and above currently available measures.
METHODS
Study assessmentsThis was a single-centre, prospective and non-randomised observational study approved by the local research ethics committee. Patients with colorectal liver metastases selected for curative major liver resection were recruited consecutively. Pre-operative MRI was performed at 1.5T (Siemens Aera), including DGE-MRI with an 8min free-breathing 3D spoiled gradient-echo (2.4s temporal resolution, TR/TE=2.45ms/0.76ms, FA=25°, acquisition matrix=128x77, FOV=400x400mm, reconstructed voxel size 3.125x10mm). 10mL Gadoxetate (Primovist, Bayer) was delivered at 1 mL/sec. Hepatectomies were performed using an open surgical technique, and biochemical and clinical progress was observed until discharge.
Data collection
Day 5 post-operative bilirubin was recorded as the primary outcome due to its common use as a surrogate for liver function. Pre-operative data included weight, age, diabetes status, BMI, chemotherapy use, renal insufficiency and biochemistry: bilirubin, ALT, Alkaline Phosphatase, Albumin, INR, Prothrombin time, Lactate. Evidence of liver steatosis was determined by histology.
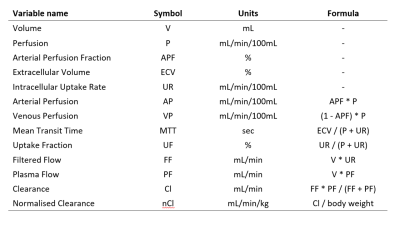
DGE-MRI processing produced 13 biomarkers for the whole liver and the FLR (Figure 1) and was performed blinded using open-source software PMI 0.4 as described previously3. Arterial- and venous input functions and a whole liver volume-of-interest (VOI) were defined semi-automatically. Liver segments were delineated using anatomical landmarks and an FLR VOI was created by joining up all segments in the FLR. Concentrations were calculated by assuming linearity with the signal and interpreted with a dual-inlet two-compartment uptake model.
Data analysis
The analysis aimed to identify which variables consistently offer useful predictions in combination with others. Prediction modelling evaluated all linear permutations of variables in a given subtype (clinical, whole liver DGE-MRI and FLR-based DGE-MRI) with the Bayesian Information Criterion. Variables consistently retained in the better fitting models were considered good candidate predictors.
RESULTS
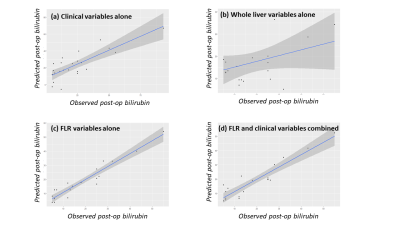
29 patients were recruited and 1 was excluded due to incomplete dynamic data collection. 15 patients had major liver resection; 8 patients underwent a more limited resection. 6 patients were deemed inoperable after MRI and excluded from analysis.Outcome predictions with best models (Figure 2) show that whole liver DGE-MRI variables alone offer poor prediction (Fig.2b), and that FLR-based DGE-MRI variables (Fig.2c) offer substantially better predictions than clinical variables (Fig.2a). Predictions do not improve when clinical variables are combined with FLR-based variables (Fig.2d), but the combination achieves good prediction with only 7 variables whereas FLR-variables alone require 11.
The 7 variables retained in the best model include one demographic variable (age), one biochemical variable (International Normalised Ratio), and 5 FLR variables: extracellular volume fraction, extracellular mean transit time, venous perfusion, filtered flow and normalised clearance. The relative weight of the FLR variables in the best model (5/7) indicates that FLR variables are most predictive. FLR volume is not retained in the best model indicating that functional measures offer better prediction.
DISCUSSION
The results offer strong indications that: (a) functional imaging substantially improves predictions of post-operative liver function over demographical and biochemical tests; (b) it is critical to measure functional variables for the FLR separately; (c) volumetry does not offer any added predictive value.The FLR variables retained in the best model reflect different aspects of liver pathophysiology. Changes in the extracellular space may reflect levels of fibrosis or liver injury, which are known risk factors for hepatectomy1. Perfusion and hepatocellular function are two components of liver function and therefore are expected to help predict post-operative function. They are both represented in the normalised clearance, an absolute measure of liver function that may offer a benchmark for what constitutes adequate post-operative liver function.
Due to the small number of observations in this pilot study the results must be treated as hypothesis generating. Stronger evidence is needed in a dataset large enough to separately provide training and testing of the idealised prediction model. The fact that 23 data points can be well fitted with a combination of only 7 variables offers confidence to justify investment in such larger studies.
CONCLUSION
DGE-MRI may substantially improve predictions of post-operative liver function over demographical and biochemical data. When confirmed in larger studies, DGE-MRI may help to reduce the risk of PHLF and potentially open up this treatment option for larger numbers of patients.Acknowledgements
This work is funded by the Medical Research Council grant reference MR/P023398/1.References
1. Kauffmann R, Fong Y. Post-hepatectomy liver failure. Hepatobiliary Surg Nutr. 2014;3(5):238–46.
2. Cieslak KP, Bennink RJ, de Graaf W, van Lienden KP, Besselink MG, Busch ORC, et al. Measurement of liver function using hepatobiliary scintigraphy improves risk assessment in patients undergoing major liver resection. HPB. 2016;18(9):773–80.
3. Sourbron S, Sommer WH, Reiser MF, Zech CJ. Combined Quantification of Liver Perfusion and Function with Dynamic Gadoxetic Acid-enhanced MR Imaging. Radiology. 2012;263(3):874–83.
Figures