2470
Liver Diffusion MRI using Optimized Gradient Waveforms, Free-Breathing Acquisitions, and Motion-Corrected Averaging: Validation in Patients1Department of Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Medical Physics, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Diffusion weighted imaging (DWI) of the liver has multiple important applications in the assessment of liver disease, including cancer. However, liver DWI faces several major challenges including signal dropout due to cardiovascular pulsation, mis-registration due to respiratory motion, and low SNR. We have developed a DWI technique that addresses these challenges by combining motion-robust diffusion waveforms to address cardiovascular pulsation, high SNR from non-gated free-breathing acquisitions, and motion-corrected averaging for respiratory motion-correction. This technique was evaluated in patients with known or suspected liver metastases. The proposed technique has the potential to enable improved assessment of liver lesions.
Introduction
Diffusion-weighted imaging (DWI) of the liver has an important role in the assessment of liver disease, including the detection, characterization, and treatment monitoring of cancer1,2. Furthermore, DWI has shown excellent promise to monitor metastatic liver lesions3. Importantly, the potential of liver DWI lies in the ability to visualize focal lesions throughout the entire liver. However, several major challenges in liver DWI need to be addressed, including signal voids introduced by cardiovascular pulsation, blurring and mis-registration due to respiratory motion, and low SNR4. To address these challenges, we had developed, and evaluated in healthy volunteers, a novel free-breathing (FB) DWI technique that combines motion-robust diffusion waveforms5,6 (to address cardiovascular pulsation) with motion-corrected averaging (to correct for respiratory motion) using a non-local means algorithm (NLM)7. In this study, we validated this technique in patients with known or suspected liver metastases.Methods
After IRB approval and informed written consent, eight patients with known or suspected liver metastases were recruited and scanned at 3T (GE Signa Premier) using flexible receive coils (AIR Technology, GE Healthcare, Waukesha, WI). A T2-weighted fast spin echo acquisition was obtained for anatomical reference. A motion-robust M1-optimized diffusion gradient waveform (MODI)5 was used to acquire DWI (b=50, 500 s/mm2) of the liver in FB without gating or triggering, using acquisition parameters shown in Table 1. An NLM-based algorithm (Fig.1) was used to address motion across repetitions and diffusion directions for each slice and each b value. Within NLM, a patch-based8 reference selection step accounted for non-rigid motion in the through-plane direction. For each slice and b value, a set of reference images was obtained by stitching together co-registered overlapping patches from all repetitions. Each reference patch was chose based on a similarity metric (mutual information) across repetitions and b values.Additionally, respiratory bellows signals from each FB acquisition were recorded to perform retrospective gating with 33% acceptance window, as an alternative reconstruction method for comparison with the proposed non-gated method. Two technical components were assessed: respiratory-motion mitigation (retrospective gating vs. non-gated FB); and signal averaging (direct averaging vs. NLM). For each respiratory-motion mitigation and signal averaging method, DW images and corresponding ADC maps were generated. Performance comparisons included: SNR of retrospective gating vs. FB images under comparable scan times, and motion-robustness of direct averaging vs. NLM via visual assessment.
Results
Data were acquired and processed successfully for all 8 patients. In this abstract, three representative examples are shown. DW images and ADC maps of a liver metastatic lesion from pancreatic cancer, processed with direct averaging, retrospective gating, and motion-corrected averaging (NLM) are shown in Fig.2. The lesion appeared extended in size with blurred boundaries in DW images and ADC maps processed with direct averaging and retrospective gating. With NLM, the shape and size of the lesion more closely match the co-localized T2-weighted acquisition, and the boundaries appeared clearer in both DW images and ADC map. Retrospective gating demonstrated lower SNR and residual respiration-related blurring and mis-registration.DW images and ADC maps of multiple liver metastatic lesions from pancreatic cancer are shown in Fig.3. The two lesions indicated by yellow arrows appeared to have blurred boundaries in DW images and ADC maps processed with direct averaging and retrospective gating. With NLM, the boundaries were clearly delineated and showed improved correspondence with the co-localized T2-weighted slice. However, despite the improved performance, NLM did not align every lesion correctly (see orange arrows).
DW images and ADC maps of an ablation site from previous treatment of hepatocellular carcinoma are shown in Fig.4. The lesion appeared extended in size with blurred boundaries in DW images and ADC maps processed with direct averaging and retrospective gating. With NLM, the shape and size of the lesion demonstrate improved correspondence with the co-localized T2-weighted slice, and the boundaries appeared clearer in both DW images and ADC map. Retrospective gating had lower SNR and residual respiration-related blurring and mis-registration.
Discussion
The patient study has demonstrated the feasibility of the proposed FB DWI technique in patients with liver lesions. This technique combines motion-robust gradient waveforms (MODI) with FB acquisitions and motion-corrected averaging in order to enable liver DWI without motion artifacts and with high SNR. The proposed NLM approach has the potential to correct for respiration-related artifacts and better align lesions within each slice and b value, and across b values. The more accurate visualization of the shape, size, and boundaries of liver lesions in both DW images and ADC maps using NLM may have important implications in the clinic and in further clinical research.This study has several limitations. Further optimization and characterization of proposed technique are desirable. The patch-based reference selection in NLM can be improved for patients with different lesion sizes and levels of DWI signal. Additionally, all lesions analyzed in this work were located in the right liver lobe; lesions in the left liver lobe need be studied to test whether MODI can address cardiac-related signal dropout. Validation of the technique in a larger patient cohort is needed in future work. In summary, the proposed motion-corrected FB DWI method shows the potential to improve image quality (i.e., motion robustness and improved SNR) compared to current methods for liver DWI.
Acknowledgements
The authors would like to acknowledge research support from GE Healthcare and Bracco Diagnostics to the University of Wisconsin-Madison. The authors also thank Juliette M. Schefelker for assistance with patient recruitment.References
[1] Koh, D. M., & Collins, D. J. (2007). Diffusion-weighted MRI in the body: applications and challenges in oncology. American Journal of Roentgenology, 188(6), 1622-1635.
[2] Gourtsoyianni, S., Papanikolaou, N., Yarmenitis, S., Maris, T., Karantanas, A., & Gourtsoyiannis, N. (2008). Respiratory gated diffusion-weighted imaging of the liver: value of apparent diffusion coefficient measurements in the differentiation between most commonly encountered benign and malignant focal liver lesions. European radiology, 18(3), 486-492.
[3] Heijmen, L., ter Voert, E. E., Nagtegaal, I. D., Span, P., Bussink, J., Punt, C. J., ... & van Laarhoven, H. W. (2013). Diffusion-weighted MR imaging in liver metastases of colorectal cancer: reproducibility and biological validation. European radiology, 23(3), 748-756.
[4] Kim, T., Murakami, T., Takahashi, S., Hori, M., Tsuda, K., & Nakamura, H. (1999). Diffusion-weighted single-shot echoplanar MR imaging for liver disease. American journal of roentgenology, 173(2), 393-398.
[5] Zhang, Y., Peña‐Nogales, Ó., Holmes, J. H., & Hernando, D. (2019). Motion‐robust and blood‐suppressed M1‐optimized diffusion MR imaging of the liver. Magnetic resonance in medicine, 82(1), 302-311.
[6] Peña‐Nogales, Ó., Zhang, Y., Wang, X., de Luis‐Garcia, R., Aja‐Fernández, S., Holmes, J. H., & Hernando, D. (2019). Optimized Diffusion‐Weighting Gradient Waveform Design (ODGD) formulation for motion compensation and concomitant gradient nulling. Magnetic resonance in medicine, 81(2), 989-1003.
[7] Geng, R., Zhang, Y., Luo, H., & Hernando, D. Toward a high-SNR, motion-robust diffusion MRI of the liver using optimized gradient waveforms, non-gated free-breathing acquisitions, and motion-corrected averaging. The 27th Annual Meeting & Exhibition of the International Society for Magnetic Resonance in Medicine. Montreal, QC, Canada, 2019. Abstract Number: 0772.
[8] Alkinani, M. H., & El-Sakka, M. R. (2017). Patch-based models and algorithms for image denoising: a comparative review between patch-based images denoising methods for additive noise reduction. EURASIP Journal on Image and Video Processing, 2017(1), 1-27.
Figures
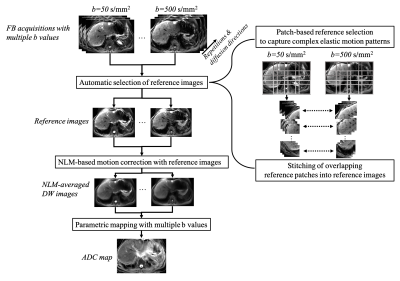
Fig.1. Workflow of NLM implementation for DWI for each slice and b value. NLM addressed motion across repetitions and directions for each b value. For each slice and b value, a set of reference images was obtained by stitching together co-registered patches from all repetitions. Each reference patch was chosen based on a similarity metric to the other repetitions and across b values. NLM averaged remaining repetitions using Gaussian-fitted weights based on local Euclidean distance to the reference images. ADC maps were calculated from the NLM-averaged images at different b values.
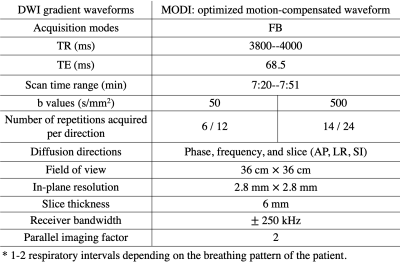
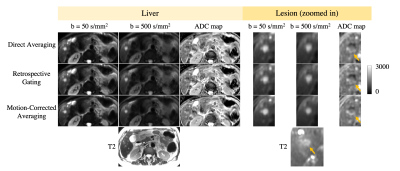
Fig.2. DW images and ADC maps of a liver metastatic lesion from pancreatic cancer, processed with direct averaging, retrospective gating, and motion-corrected averaging (NLM). The lesion appeared extended in size with blurry boundaries in DW images and ADC maps processed with direct averaging and retrospective gating, due to inadequate alignment of the lesion across repetitions and b values. And retrospective gating had lower SNR. With NLM, shape and size of the lesion showed improved correspondence to co-localized T2 reference, and boundaries appeared clearer in DWI and ADC map.
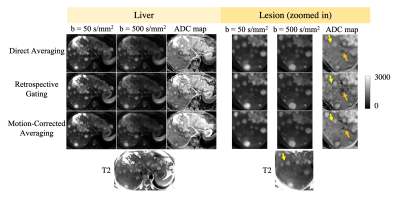
Fig.3. DW images and ADC maps of multiple liver metastatic lesions from pancreatic cancer processed with direct averaging, retrospective gating, and motion-corrected averaging (NLM). Two lesions (see yellow arrows) had blurry boundaries in DW images and ADC maps processed with direct averaging and retrospective gating. With NLM, boundaries were clearly delineated and showed improved correspondence to co-localized T2 reference. In this challenging case, NLM did not align every lesion correctly across b-values, as in a black crescent due to mis-registration (see orange arrows).
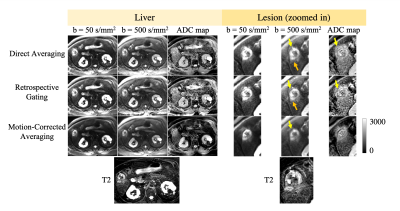
Fig.4. DW images and ADC maps of an ablation site for hepatocellular carcinoma, processed with direct averaging, retrospective gating, and motion-corrected averaging (NLM). The lesion appeared extended in size with blurry boundaries in DW images and ADC maps processed with direct averaging and retrospective gating, due to inadequate alignment of the lesion across repetitions and b values. Retrospective gating had lower SNR. With NLM, the shape and size of the lesion showed better correspondence to co-localized T2 reference, and boundaries appeared clearer in DW images and ADC map.