2438
Reduced field-of-view versus conventional pelvic diffusion-weighted imaging in rectal cancer1Department of Radiology, Stanford University, Stanford, CA, United States
Synopsis
There is growing literature supporting the use of diffusion weighted imaging (DWI) for staging and re-staging of rectal cancer. We investigated the performance of reduced FOV (rFOV) DWI in comparison with conventional whole pelvis DWI. Two readers graded rFOV and conventional DWI for anatomic detail, lesion conspicuity, tumor margin delineation, artifact, and overall image quality. rFOV DWI showed statistically significant improvement in anatomic detail, lesion conspicuity, tumor margin delineation, and overall image quality. No significant difference in artifact/distortion or lymph nodes was detected. rFOV DWI is a promising technique in rectal cancer evaluation and improves tumor visualization.
INTRODUCTION
MR imaging is the preferred diagnostic modality in the local staging and re-staging of rectal cancer1. Although primary evaluation of rectal cancer is made on high-resolution T2-weighted imaging of the rectum as well as post-contrast imaging, there has been increasing evidence in recent years regarding the utility of diffusion weighted imaging (DWI)2. The combination of DWI and T2-weighted imaging has been shown to provide both excellent detection of primary rectal tumors3,4 and improved diagnostic performance when evaluating for treatment response after neoadjuvant chemoradiation (CRT)5–7 compared to T2-weighted imaging alone. Recent years have also seen a growth in the application of reduced field-of-view (rFOV) diffusion techniques in the pelvis, including the cervix8 and prostate9, to provide high spatial resolution DWI of small organs of interest while minimizing image distortion. This study was performed to evaluate the image quality of a rFOV DWI pulse sequence with conventional DWI covering the whole pelvis in the setting of rectal cancer staging.METHODS
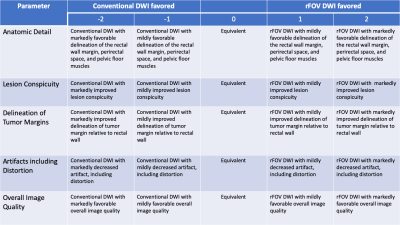
This prospective study was performed on 18 consecutive patients that had MRI performed for evaluation of rectal cancer. 7 patients were scanned for primary evaluation and 11 were performed for re-staging after CRT. All images were obtained on a 3.0T MR system (Discovery MR750, GE Healthcare, Waukesha, WI) with a 32 channel phased-array coil. Patients were administered 1 mg of intramuscular glucagon prior to examination to reduce bowel motion artifact and ultrasound gel was instilled in the rectum to facilitate delineation of rectal tumors. rFOV DWI was obtained using a 2D spatially selective RF pulse and echo-planar readout (FOV optimized and constrained undistorted single shot [FOCUS], GE Healthcare, WI) with a FOV of 24 x 14.4 cm. Conventional DWI was obtained with a spectral-spatial RF pulse with an echo-planar readout at an FOV of 40 x 40 cm. The echo time and repetition time were optimized for each patient based on scan coverage, with typical parameters of TE = 65 ms/TR = 9500 ms for rFOV DWI and TE = 61 ms/TR = 15500 ms for conventional DWI. The remainder of imaging parameters were conserved between both diffusion protocols (Slice thickness = 3 mm, Slice skip = 0 mm, Flip angle = 90, Matrix = 128x80, b-value = 50 and 1000, Number of signal averages at high b-value = 14, typical acquisition time of approximately 2-2.5 minutes).Image quality was assessed by board-certified (V.S.) and board-eligible (A.J.) radiologists using a 5-point scale to determine preference for anatomic detail, lesion conspicuity, tumor margin delineation, distortion, and overall image quality. The number of perirectal, pelvic sidewall, and inferior mesenteric lymph nodes were also counted in each series. Images were reviewed in conjunction with T2-weighted and contrast-enhanced sequences. Readers were not blinded to the DWI sequence in question as readily apparent differences in the images made blinding impractical. However, readers were blinded to clinical history. Statistical significance for difference in image quality was evaluated using the two-sided Wilcoxon signed rank test with Bonferroni-Holm correction for multiple comparisons with α = 0.05. Statistical significance for the difference in the number of lymph nodes detected was performed using a two sample t-test with α = 0.05. Statistics were calculated using the R statistical package in RStudio desktop (RStudio, Boston, MA).
RESULTS
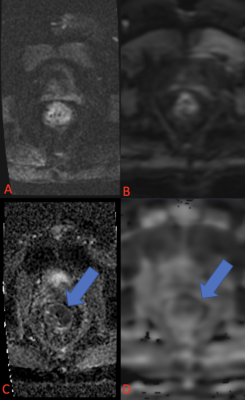
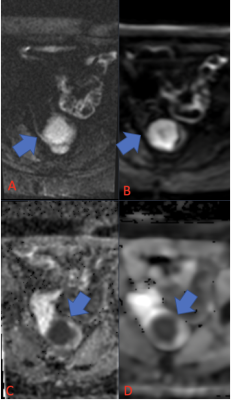
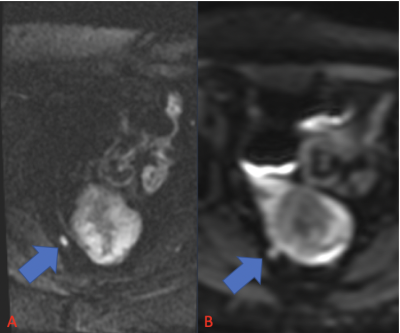
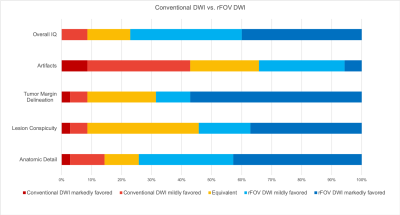
For both readers, rFOV DWI provided significantly increased anatomic detail (mean = 1.01, p= 0.003), lesion conspicuity (mean = 0.80, p = 0.012), tumor margin delineation (mean = 1.14, p= 0.0001), and overall image quality (mean = 1.08, p= 0.0002) compared to conventional DWI. Artifact, including distortion, was slightly more noticeable in rFOV DWI although this difference was not statistically significant (mean = -0.11, p= 0.54). The weighted Cohen’s kappa statistic for all observations was 0.40, indicating fair agreement between the two readers. There was no significant difference in the number of lymph nodes detected (p= 0.22).DISCUSSION
Our study suggests that rFOV DWI provides preferable visualization of anatomic detail, lesions, tumor margins, and overall image quality compared to conventional DWI, without significant difference in distortion or artifact. DWI has been shown to be a useful diagnostic adjunct to high-resolution T2-weighted imaging in the rectum particularly in cases assessing for tumor response to chemoradiation therapy7. rFOV DWI allows for higher spatial resolution and improved image quality and therefore should be considered in rectal cancer imaging protocols. This study has several limitations: only 18 patients were assessed – data on a larger cohort of patients is warranted. Our study also did not assess pathologic correlation of findings on DWI. As has been reported previously, restricted diffusion can be seen in fibrotic tissue after CRT6. Further investigation is needed to determine if rFOV DWI provides similar, better, or worse performance when correlated with histopathology.CONCLUSION
rFOV DWI provides preferable delineation of anatomic detail, rectal tumor margin, lesion conspicuity, and overall image quality compared to conventional DWI in rectal cancer staging and re-staging. rFOV DWI did not introduce significant artifact or distortion compared to conventional DWI. rFOV DWI provides superior diffusion-weighted evaluation of the rectum in rectal cancer and its inclusion in rectal cancer imaging protocols should be considered.Acknowledgements
The authors would like to acknowledge Andreas Loening and Ryan Brunsing for their assistance in abstract preparation.References
1. Beets-Tan RGH, Lambregts DMJ, Maas M, et al. Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2018;28(4):1465-1475. doi:10.1007/s00330-017-5026-2
2. Schurink NW, Lambregts DMJ, Beets-Tan RGH. Diffusion-weighted imaging in rectal cancer: current applications and future perspectives. Br J Radiol. 2019;92(1096):20180655. doi:10.1259/bjr.20180655
3. Soyer P, Lagadec M, Sirol M, et al. Free-breathing diffusion-weighted single-shot echo-planar MR imaging using parallel imaging (GRAPPA 2) and high b value for the detection of primary rectal adenocarcinoma. Cancer Imaging. 2010;10(1):32-39. doi:10.1102/1470-7330.2010.0011
4. Rao S-X, Zeng M-S, Chen C-Z, et al. The value of diffusion-weighted imaging in combination with T2-weighted imaging for rectal cancer detection. Eur J Radiol. 2008;65(2):299-303. doi:10.1016/j.ejrad.2007.04.001
5. van der Paardt MP, Zagers MB, Beets-Tan RGH, Stoker J, Bipat S. Patients Who Undergo Preoperative Chemoradiotherapy for Locally Advanced Rectal Cancer Restaged by Using Diagnostic MR Imaging: A Systematic Review and Meta-Analysis. Radiology. 2013;269(1):101-112. doi:10.1148/radiol.13122833
6. van der Sande ME, Beets GL, Hupkens BJP, et al. Response assessment after (chemo)radiotherapy for rectal cancer: Why are we missing complete responses with MRI and endoscopy? Eur J Surg Oncol. 2019;45(6):1011-1017. doi:10.1016/j.ejso.2018.11.019
7. Lambregts DMJ, Vandecaveye V, Barbaro B, et al. Diffusion-Weighted MRI for Selection of Complete Responders After Chemoradiation for Locally Advanced Rectal Cancer: A Multicenter Study. Ann Surg Oncol. 2011;18(8):2224-2231. doi:10.1245/s10434-011-1607-5
8. Hwang J, Hong SS, Kim H-J, et al. Reduced field-of-view diffusion-weighted MRI in patients with cervical cancer. Br J Radiol. 2018;91(1087):20170864. doi:10.1259/bjr.20170864
9. Ma S, Xu K, Xie H, et al. Diagnostic efficacy of b value (2000 s/mm2) diffusion-weighted imaging for prostate cancer: Comparison of a reduced field of view sequence and a conventional technique. Eur J Radiol. 2018;107:125-133. doi:10.1016/j.ejrad.2018.08.028
Figures