2435
Comparative study of APT combined with DKI in post-chemotherapy and non-chemotherapy rectal cancer
Xuedong Wang1, Anliang Chen1, Qingwei Song1, Jiazheng Wang2, and Ailian Liu1
1The first affiliated hospital of dalian medical university, DaLian, China, 2Philips Healthcare, China, Beijing, China
1The first affiliated hospital of dalian medical university, DaLian, China, 2Philips Healthcare, China, Beijing, China
Synopsis
We aimed to explore the difference of amide proton transfer-weighted (APTw) imaging combined with DKI between the chemotherapy group and non-chemotherapy group of rectal cancer. The result showed that the highest diagnostic efficacy(AUC: 0.986; sensitivity: 91.8%; specificity: 100%) was acquired using APT combined with DKI, rather than APT and DKI value respectively.
Introduction
Rectal cancer is the third most common cancer and the second cause of cancer-related death worldwide[1], and preoperative chemotherapy were often used on cancer of high stage before surgury. The assessment of there sponse to chemotherapy is hence a matter of great clinical concern.Due to the need to evaluate its chemotherapy effect with multiple times, a non-invasive technique is needed to evaluate the composition and activity of the lesion. Amide proton transfer-weighted (APTw) imaging as an endogenous chemical exchange saturation transfer (CEST) imaging technique can assess the changes in the intracellular protein concentration and PH by detecting the proton exchange between the amide protons in endogenous mobile proteins and bulk-water protons, and it has been applied in different disease and organs [2-4]. Diffusion kurtosis imaging (DKI) is developed on the basis of diffusion tensor imaging (DTI),measuring the dispersion of water in the anisotropic restricted environment[5]. The purpose of this study was to investigate the difference of quantitative APTw and DKI imaging in chemotherapy group and non-chemotherapy group of rectal cancer, which may provide a clinical tool to measure the chemotherapy response in the future.Materials and Methods
This study has been approved by the local IRB. Images of 18 patients with rectal cancer in our hospital were retrospectively analyzed, including 6 cases of post-chemotherapy lesions and 12 cases before chemotherapy. For all the cases, ATPw, DKI and Conventional MRI scan(including T1W,T2W, DWI and DCE)were performed on a 3.0T MR scanner (Ingenia CX, Philips Healthcare, Best, the Netherlands) (Table 1).Images were analyzed on a post-processing workstation (Intellispace Portal;v. 10.1.0.64190; Philips Healthcare, Best, the Netherlands). Referring to theanatomical location of lesion obtained on T2-weighted, DWI and DCE images (Figure 1),three circle ROIswere manually placed on the largest lesions on APTw and DKI(FA、MD、MK) parameter images, respectively.ATP values [4] and DKIparameterwere measured and the average values were used to compared between the two groups by using Mann-Whitney U test. ROC curvesof the above parameters were used to analyze quantitativevalues changes of chemotherapy and non-chemotherapyof rectal cancer lesions. Logistic regression was also used to calculate the value of APT combined with DKI parameters.Result
The median (25th Percentile, 75th Percentile) of APT value (%) for chemotherapy group were 2.25 (1.82, 2.35), lower than non-chemotherapy group2.88 (2.32, 3.18)(p<0.05). Yetthe median (25th Percentile, 75th Percentile) of MD value (μm2/ms) for chemotherapy group were 1.22 (1.02, 2.48), higher than non-chemotherapy group0.72 (0.67, 0.92)(p<0.05). FA and MK value of DKI were no significant difference in chemotherapy group and non-chemotherapy group. Area under the curve (AUC) for APT and MD values to differentiate chemotherapy and non-chemotherapy group lesions were 0.875 and 0.819 respectively. The sensitivity and specificity of above parameters corresponding to their respective feasible threshold values were100% and 75% of APT,83.3% and 83.3%of MD value. With APT values combined with MD values in the chemotherapy and non-chemotherapy of rectal cancer, we found thatthe diagnostic efficacy was significantly higher (AUC=0.986), as well as the sensitivity of 100% and the specificity of 91.7% (Figure 2).Discussion and conclusion
APTw imaging combined and DKI can reflect the difference in lesion characteristicsof rectal cancer with and without chemotherapy. Because tumor cells have a high proliferative activity and the hence up regulated protein synthesis, and chemotherapy is usually aimed at high-proliferative cells, the APT values of chemotherapy group were lower than non-chemotherapy group.Due to the increase infree water and inflammatory cell infiltration in the lesion after chemotherapy,the MD value of chemotherapy group were larger than non-chemotherapygroup. This finding, if confirmed with a study under-planning with larger sample size, has the potential to provide a guidance for the chemotherapy as an assessment tool for therapy outcome.Acknowledgements
no acknowledgements foundReferences
[1] Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017[J]. Ca A Cancer Journal for Clinicians, 2017, 67:104-117. [2] Zhou Jinyuan, HeoHye-Young, Knutsson Linda, et al. APT-weighted MRI: Techniques, current neuro applications, and challenging issues[J]. MagnResonFigures
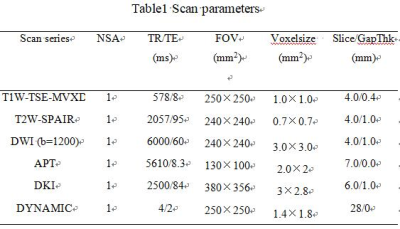
Table1 Scan
parameters
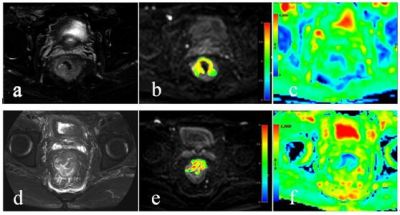
Figure
1 A 77-year-old male patient with chemotherapy
of rectal cancer. T2W
image (a), APTw-DWI fusion image (b)and MD image (c)to showthe lesion of rectal
cancer with chemotherapy. The average of APT and MD values were 1.79% and 2.38μm2/ms.A 65-year-old
male patient with chemotherapy of rectal
cancer. T2W image (d), APTw-DWI fusion image (e)and MD
image (f)to showthe lesion of rectal cancer with chemotherapy. The average of APT and
MD values were 4.07% and 0.706μm2/ms.
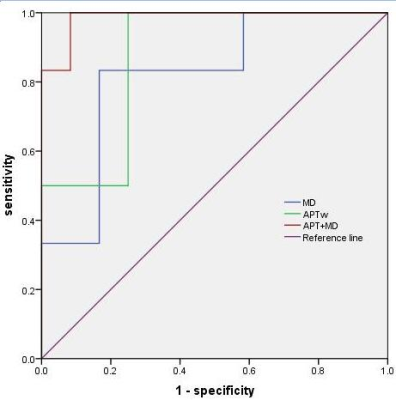
Figure2. ROC
Curves of APT and MD value as well as APT value combined MD value in the
comparison of chemotherapy and
non-chemotherapy of rectal cancer. The significantly high (AUC=0.986) of
diagnostic efficacy wasacquired with combination of APT and MD values with the
sensitivity of 100% and the specificity of 91.7%.