2431
R2* relaxation rates of pelvic lymph nodes in USPIO-enhanced MRI of rectal cancer patients at 3 and 7T1Radiology and Nuclear Medicine, Department of Surgery, Radboudumc, Nijmegen, Netherlands, 2Radiology and Nuclear Medicine, Radboudumc, Nijmegen, Netherlands
Synopsis
Six patients with rectal cancer underwent USPIO-enhanced MRI at 3 and 7T. The presence and appearance of lymph nodes was annotated by two trained radiologists. Lymph nodes were matched between 3 and 7T, and ROIs were drawn inside the nodes to calculate mean R2* relaxation rates in order to assess the possibilities of quantitative thresholds in R2* between suspicious and benign lymph nodes at both field strengths.
Introduction
In management of rectal cancer, lymph node staging determines treatment regimens and has prognostic implications. In order to optimize non-invasive nodal staging, USPIO-enhanced MRI could aid in the detection of metastatic lymph nodes, as several studies in prostate cancer have shown (1, 2). Recently, the feasibility of the use of USPIO-enhanced 7T MR imaging has been demonstrated in prostate and rectal cancer staging (3). USPIO nanoparticles, administered intravenously one day before MR imaging, accumulate in healthy lymph nodes, reflecting hypointense signal on T2*-weighted imaging. On the contrary, suspicious lymph nodes will reflect a hyperintense MR signal. The sensitivity of MR at 7T in combination with the TIAMO technique allows 3D GRE imaging of the whole pelvis at unprecedented spatial resolution (4). To assess and quantify the appearance of benign and suspicious lymph nodes we compared R2* relaxation rates of these nodes in patients with rectal cancer examined both at 3 and 7T.Methods
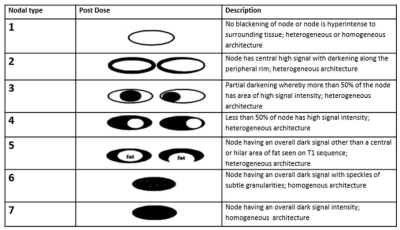
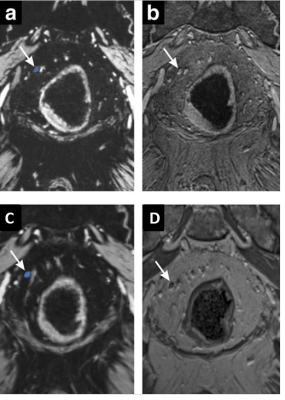
Six patients with rectal cancer were examined in a prospective observational pilot study to assess the added value of USPIO-enhanced MR imaging on 3- and 7T. All patients underwent a 3T and a 7T MR examination on the same day (Prisma and Magnetom 7T, Siemens), 24–36 h after an intravenous infusion of USPIOs (ferumoxtran-10, SPL Medical B.V, Arnhem, the Netherlands) of 2.6-mg iron per kg of bodyweight. Two sequences (anatomical and MGRE R2*-weighted) were used on both 3 and 7 T. Protocol parameters 7T: MGRE resolution 0.68mm3 isotropic, TR=16ms, flip angle≈16°, TEs 2.28ms, 4.76ms, 7.24ms, 9.72ms, 12.20ms; GRE anatomical imaging 0.68mm3 isotropic, TR=5.9ms, flip angle≈21°. Protocol parameters 3T: MGRE resolution 0.85mm3 isotropic, TR=21ms, flip angle=10°, TEs 3.60ms, 7.00ms, 10.40ms, 13.80ms, 17.20ms; GRE T1W imaging 0.9mm3 isotropic, TR=5.8ms, flip angle=10°. Detection of lymph nodes was done on T1-weighted MRI and on multi-gradient echo T2*-weighted MRI with reconstructed computed echo time of 12msec (3). USPIO-enhanced MR images were evaluated by 2 experienced radiologists, using a classification scheme as illustrated in table 1 and annotated accordingly using MevisLab (MeVis Medical Solutions AG, Bremen, Germany). Nodal type 1-3 was considered suspicious and type 5-7 was considered unsuspicious. Where possible, lymph nodes on 3 and 7T MR imaging were matched for comparison. Regions of interest (ROI) were drawn around all annotated lymph nodes using MevisLab. A computed echo time of 0 ms was used to draw the ROI, shown in figure 2. These ROI’s were transferred to the image sets at different echo times to assess the mean signal intensity decay of the ROI. The mean signal intensities of lymph nodes per echo time were used to calculate R2* relaxation rates of the nodes at both field strengths (GraphPad Prism, San Diego California USA, www.graphpad.com) with a weighted non-linear mono-exponential fit. Because magnitude signal intensities induce Rician noise, we estimated non-zero plateau signal intensities for 3T and 7T in a first fitting round, and included them as prior knowledge to the equation to perform a second R2* fit. Fitted R2* relaxation rates with an R-square above 0.90 were considered appropriate, and were compared between field strengths and radiological classifications on T2*weighted imaging. A one-way ANOVA was performed to evaluate whether differences in R2* relaxation rates were patient dependent.Results
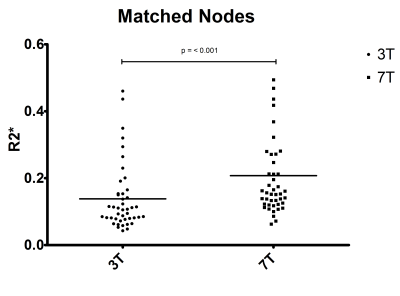
In six patients MGRE imaging at both field strengths was successfully performed. A total of 44 lymph nodes from 5 patients could be matched, e.g. they were identified by both radiologists, and they were visible on cTE = 0ms images at both 3 and 7T. The distributions of R2* relaxation rates of lymph nodes visible on 3 and 7T imaging differed significantly (P < 0.001) (Fig. 3). Mean R2* relaxation rate of the lymph nodes at 3T was 0.14 ms-1 (corresponding to T2* of 7.1 ms) and 0.21 ms-1 (corresponding to T2* of 4.8 ms) of the 7T lymph nodes. Comparing the nodes in matched pairs, the R2* of 29 nodes increased, 6 nodes decreased (all from one patient), and 3 nodes remained unchanged (Fig. 4A/B) from 3 to 7T. Suspicious nodes have longer R2* than nodes that appear benign. After performing a one-way ANOVA, R2* relaxation rates of suspicious lymph nodes on both 3T (P<0.001) and 7T (P=0.03) imaging were significantly different between patients.Discussion
In this work we report on quantitative R2* relaxation rates of USPIO enhanced lymph nodes in rectal cancer on 3 and 7T MR imaging. Although R2* is a parameter that can depend on many different factors, we assumed that the introduction of USPIO nanoparticles had the strongest influence on the exact value of the R2* in the lymph nodes. When nodes are selected on the basis of appearance on T2*-weighted MRI with cTE = 12 ms (suspicious or benign), it is obvious this distinction is reflected in different R2* values. Histopathological validation of detected nodes is needed in future work.Conclusion
Significant differences in R2* of lymph nodes in USPIO-enhanced MRI between patients, and the large increase in R2* in matched nodes when moving from 3 to 7T can provide a more quantitative handle on the level of suspicion of the nodes containing metastases.Acknowledgements
No acknowledgement found.References
1. Harisinghani MG, Barentsz J, Hahn PF, Deserno WM, Tabatabaei S, van de Kaa CH, et al. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med. 2003;348(25):2491-9.
2. Heesakkers RA, Hovels AM, Jager GJ, van den Bosch HC, Witjes JA, Raat HP, et al. MRI with a lymph-node-specific contrast agent as an alternative to CT scan and lymph-node dissection in patients with prostate cancer: a prospective multicohort study. Lancet Oncol. 2008;9(9):850-6.
3. Philips BWJ, Stijns RCH, Rietsch SHG, Brunheim S, Barentsz JO, Fortuin AS, et al. USPIO-enhanced MRI of pelvic lymph nodes at 7-T: preliminary experience. Eur Radiol. 2019.
4. Orzada S, Maderwald S, Poser BA, Bitz AK, Quick HH, Ladd ME. RF excitation using time interleaved acquisition of modes (TIAMO) to address B1 inhomogeneity in high-field MRI. Magn Reson Med. 2010;64(2):327-33.
Figures
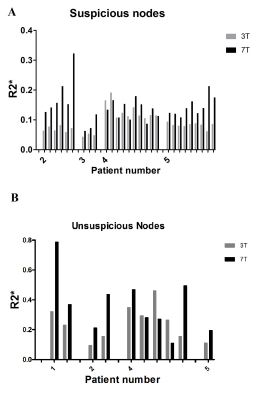
4B: R2* relaxation rates of all paired unsuspicious lymph nodes