2429
A preliminary study of 3D-amide proton transfer MR imaging in rectal adenocarcinoma: comparison with diffusion kurtosis imaging
Weicui Chen1, Ling Li2, Yingjie Mei3, Jilei Zhang3, Weikang Huang1, Bo Liu1, and Xian Liu1
1Radiology, The second Affiliated hospital of Guangzhou University of Chinese Medicine, Guangzhou, China, 2Guangzhou University of Chinese Medicine; The second Affiliated hospital of Guangzhou University of Chinese Medicine;, Guangzhou, China, 3Clinical Science,Philips Healthcare;, Shanghai, China
1Radiology, The second Affiliated hospital of Guangzhou University of Chinese Medicine, Guangzhou, China, 2Guangzhou University of Chinese Medicine; The second Affiliated hospital of Guangzhou University of Chinese Medicine;, Guangzhou, China, 3Clinical Science,Philips Healthcare;, Shanghai, China
Synopsis
We explore the utility of 3D APTw imaging and DKI in assessing the pathological factors of rectal adenocarcinoma. The mean APTSI and MK was higher with the advanced staging and grading in rectal adenocarcinoma. In addition, the mean APTw SI have a significantly positive correlation with WHO grades. Therefore, the mean APTw SI is promising to be a non-invasive biomarker in clinical practice and to become a potential predictor for estimating the prognosis of rectal adenocarcinoma.
Purpose and Introduction
Rectal Adenocarcinoma is a common cause of cancer-related mortality and morbidity, especially in the developed countries1. According to the evaluation of the grade and stage in rectal carcinoma, the treatment protocols are usually surgery and /or neoadjuvant chemoradiation therapy2. Conventional MR imaging have been proven significantly assessed the anatomical characteristics, such as tumor invasion depth, lymph nodal stage and extramural venous invasion. The functional MR imaging in clinical including diffusion-weighted MR imaging, dynamic-contrast enhanced MRI etc., could reflect the physiological information of tumor. However, the analysis of anatomic, mono-exponential and non- gaussian model in tumors is not enough to guide the treatment strategy. Amide proton transfer (APT) MR imaging is based on chemical exchange saturation transfer (CEST) processes and could provide molecular information of cell density and the amide protons (-NH groups) of endogenous mobile protein/peptides, which helps the evaluation of tumor grading and differential information3. We aim to investigate the feasibility of 3D APTw imaging in predicting pathologic factors for rectal adenocarcinoma, in comparison with diffusion kurtosis imaging (DKI).Materials and Methods
Sixty-three rectal adenocarcinoma patients were included in this study. MR examinations were performed using a 3.0T MR scanner (Ingenia, Philips Healthcare, Best, the Netherlands) with 32- channel phase array coil. MR scanning protocol included T1-weighted imaging (T1WI), T2-weighted imaging(T2WI), 3D-TSE-APT imaging, DKI and dynamic contrast-enhanced T1WI. APTw imaging and DKI were performed before the administration of gadolinium diethylenetriaminepentaacetic acid (Gd-DTPA, Bayer HealthCare, Guangzhou, China). APT weighted signal intensity was defined as the magnetization transfer asymmetry (MTRasym) at 3.5ppm, and displayed as percentage level APTw%, APTw%=MTRasym [Δɷ=+3.5 ppm] (%). DKI (with b values of 0, 600, 1000, and 2000 sec/mm2) was performed using a single shot echo-planar (SS-EPI) sequence and mean kurtosis (MK) and mean diffusivity (MD) maps were obtained. ADC value was calculated based on DWI data with b value of 0 and 1000sec/mm2. The mean APTw SI, MK, MD and ADC values were calculated by averaging signal intensities measured on all slices. Tumor pathological analysis included WHO grades, pT stages, pN stages. Mean APTwSI, MK, MD and ADC mean were compared between different groups using Student’s t- test and one way-ANOVA. Spearman correlation was used for correlation analysis between MR parameters and tumor T stages. Receiver-operating characteristics (ROC) analysis was performed to evaluate diagnostic performance of these different MR parameters for differentiating low grade from high grade rectal adenocarcinoma.Results
The inter-observer agreement was excellent between two observers for APT, MK, MD and ADC values. According to the World Health Organization (WHO) classification of colorectal carcinoma, high-grade rectal adenocarcinoma showed significantly higher mean APTw SI and MK values. Low grade and high grade tumors showed no difference in MD (1.216±0.174×10-3mm2/s vs1.156±0.131×10-3mm2/s, p=0.62), and ADC values (1.086±0.146×10-3mm2/s vs1.045±0.08×10-3mm2/s, p=0.254). Rectal adenocarcinoma in the T4 stage demonstrated higher mean APTw SI than that of T2, T3 stages. For MK, there is a significant difference between T2 and T4 stage, T3 and T4 stage, while no difference between T2 and T3 stage rectal adenocarcinoma was detected. The MD and ADC in all rectal adenocarcinoma demonstrated no differences among T2, T3 and T4 stage. Mean APTw SI, MK were significantly higher in tumors with lymph node involvement (pN1-2) than in tumors without metastatic lymph nodes (pN0) (2.908±0.558 vs 2.183±0.521, p=0.000; 1.189±0.265 vs1.005±0.127, p=0.001 respectively). There was no significant difference in MD and ADC between pN0 and pN1-2 groups. Mean APTw SI exhibited a significantly high positive correlation with WHO grades (r=0.618, 95% confidence interval: 0.437 to 0.750). Kurtosis, diffusivity and ADC showed no correlation with WHO grades (r=0.208, 95% confidence interval: -0.0415 to 0.434; r=-0.0985, 95% confidence interval: -0.338 to 0.153; r=-0.226, 95% confidence interval: -0.448 to 0.0233, respectively). ROC analysis demonstrated using mean APTw SI had a 87.50% sensitivity and 77.42% specificity for distinguishing low grade from high grade rectal adenocarcinoma, providing a better diagnostic capacity than MK, MD and ADC mean (Figure 2). Figure 1 demonstrate representative images.Conclusion
Compared with DKI, mean APTw SI demonstrated a high correlation with rectal adenocarcinoma with different prognostic factors, exhibiting a better diagnostic capability in discriminating low- grade from high grade rectal adenocarcinoma. 3D-APT imaging is utility for the diagnose of rectal carcinoma, and has the potential to become a non-invasive biomarker.Acknowledgements
No acknowledgement found.References
1. F B, J F, I S, RL S, LA T, clinicians JAJCacjf. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. 2018; 68(6): 394-424. 2. K N, L S, Q C, et al. Rectal Cancer: Assessment of Neoadjuvant Chemoradiation Outcome based on Radiomics of Multiparametric MRI. 2016; 22(21): 5256-64. 3. H Y, X W, P W, et al. Can amide proton transfer-weighted imaging differentiate tumor grade and predict Ki-67 proliferation status of meningioma? 2019; 29(10): 5298-306.Figures
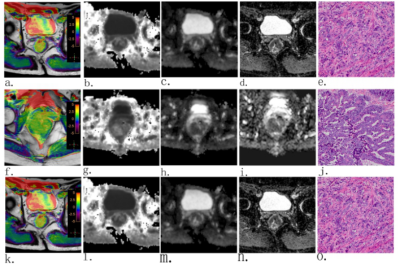
Figure1.
The well (male, a-e), moderately(female, f-j), poorly(male, k-o)differentiated
rectal adenocarcinoma. APTw-T2 merged image shows a mean APTw SI of 1.67%(a),
2.45%(f), 3.04%(k)). Kurtosis, Diffusivity and ADC maps shows high, low and low
signal intensity tumor, respectively(MK=0.882(b), 1.097(g), 1.271(l); MD=
1.373×10-3mm2/s(c), 1.287×10-3mm2/s(h);
1.159×10-3mm2/s(m); mean ADC=1.142×10-3mm2/s(d),
1.054×10-3mm2/s(i), 1.014×10-3mm2/s(n)).
H. E staining shows histopathological characters of the tumor (e, j, o)(×40).
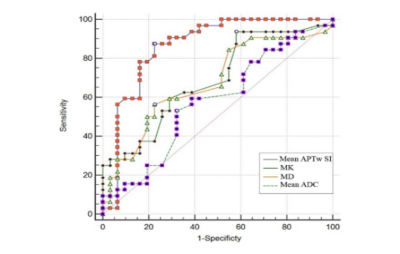
Figure
2. A comparison of the diagnostic capability for discriminating low grade from
high grade rectal adenocarcinoma between mean APTw SI, MK, MD and mean ADC. ROC
analysis shows mean APTw SI has a higher are a under the curve (0.8624) that
the other parameters.