2427
Developing Hybrid Multidimensional MRI without an endorectal coil for the detection of prostate cancer: a feasibility study1Department of Radiology, University of Chicago, Chicago, IL, United States, 2Department of Radiodiagnosis, King George's Medical University, Lucknow, India, 3Philips Research North America, Cambridge, MA, United States, 4Department of Pathology, University of Chicago, Chicago, IL, United States, 5Department of Urology, University of Chicago, Chicago, IL, United States
Synopsis
There are conflicting reports on the use of endorectal coil in the detection of prostate cancer at 3T due to increased patient discomfort and susceptibility artifacts. The purpose of the present study was to evaluate the feasibility of Hybrid Multidimensional MRI (HM-MRI) without an endorectal coil (using pelvic phased-array coil only) in the detection of prostate cancer (PCa) and to calculate fractional volumes of prostatic tissue composition, non-invasively. A non-endorectal coil HM-MRI is feasible. We obtained a significant difference in epithelium volume between normal and PCa (p = 0.02), however stromal and luminal volume did not reach a significance level.
Introduction
Changes in the relative percentages of epithelium, stroma, and lumen are expected with the presence of prostate cancer (PCa) and varying Gleason grade. We recently demonstrated that Hybrid Multidimensional MRI (HM-MRI) can measure these tissue composition changes and is useful for diagnosing prostate cancer non-invasively.1, 2 HM-MRI has shown the ability to localize, detect, and assess the aggressiveness of PCa.2 However, previous studies utilized endorectal coil in combination with a phased-array coil. There are conflicting reports on the use of endorectal coil in the detection of PCa at 3T due to increased patient discomfort, susceptibility artifacts, and cost.3-5 It would be beneficial to use the HM-MRI technique as a screening tool for PCa if this procedure is used without an endorectal coil. In the present study, we evaluate the feasibility of HM-MRI without an endorectal coil (phased-array coil only) in the detection of clinically significant PCa and to calculate fractional volumes of prostatic tissue composition, non-invasively.Methods
This IRB approved, HIPAA compliant, prospective study included 16 men with biopsy confirmed PCa (mean age: 56.8 ± 7.7 years) who signed informed consent prior to imaging. All patients underwent a preoperative MRI on a 3T whole body MRI system (Ingenia, Philips Healthcare) using a pelvic phased-array coil between March 2019 and October 2019 (ongoing study) prior to undergoing radical prostatectomy. Imaging parameters were as follows: axial 2D T2W turbo spin echo: TR/TE = 4000/110 ms, slice thickness = 3 mm, FOV = 200 X 200 mm2, matrix = 400 x 250. Coronal 2D T2W turbo spin echo: TR/TE = 4025/110 ms, slice thickness = 3 mm, FOV = 200 X 200 mm2, matrix = 400 x 250. Transverse images using HM-MRI were acquired with all combinations of TE = 70, 90, 110, 130 ms and b-values of 0, 300, 600, 900 s/mm2, and TR = 8150 ms. Fractional volumes of tissue components - epithelium, stroma, and lumen were calculated by fitting the HM-MRI data to a three-compartment signal model, with distinct, paired apparent diffusion coefficient (ADC) and T2 values associated with each compartment on a voxel-by-voxel basis, similar to the previous study. 2 The acquisition time for HM-MRI sequence was 12-15 minutes. We also acquired dynamic contrast enhanced MRI using DOTAREM (Guerbet LLC) as contrast agent and clinical diffusion weighted images, however these data were not analyzed in the current study. Histopathology was used as a reference standard. The significance of differences in mean value of various fractional volumes between normal and PCa was measured by the t-test. Receiver operating characteristic (ROC) analysis was used to evaluate the performance of various parameters in differentiating prostate cancer from normal prostatic tissue. Statistical analyses were performed using SPSS 26.0 (SPSS Inc., Chicago, IL, USA).Results
Of 16 patients, 5 were analyzed in this preliminary analysis. The patient characteristics are listed in Table 1. PCa was detected in all patients. Mean PSA was 9.7 ng/ml and median Grade Group was 3 ranging between 2 and 4. Representative images of tissue composition measured using HM-MRI showing non-invasive measurement of epithelium, stroma, and lumen fraction volume are presented in Figure 1. The mean fractional volume was 29±15% for epithelium, 56±8% for stroma, and 15±13% for lumen in PCa. The mean fractional volume was 7±4% for epithelium, 66%±11% for stroma, and 27±13% for lumen in normal prostatic tissue. We obtained a significant difference in epithelium volume between normal prostate and PCa (p = 0.02), however the differences in stromal and luminal volume fractions between PCa and normal prostate did not reach statistical significance (p = 0.1 and p = 0.2) (Table 2). The area under the ROC curve for the epithelium volume fraction in differentiating normal prostate and PCa was 0.9 (95% confidence interval, 0.7 - 1).Discussion
A recent report found that the majority of studies both at 1.5T and 3T were acquired without an endorectal coil.6 Though an endorectal coil increases signal-to-noise ratio and image quality, 4, 7 there is a growing interest in non-endorectal studies in order to avoid patient discomfort, motion artifacts, and susceptibility artifacts.3, 5 With the increasing use of MRI in biopsy naïve patients, excellent image quality is needed in conjunction with high patient comfort and acceptance. Our study shows that the HM-MRI is feasible using pelvic phased-array coil only. We were able to measure the tissue composition map using the compartmental analysis of HM-MRI that provides morphological features non-invasively. A similar trend has been observed previously in morphometric analysis of tissue composition from hematoxylin- eosin- stained prostate tissue. 8 A major strength of the study was developing a non-endorectal coil HM-MRI protocol, and calculating fractional volumes of various tissue composition non-invasively. We observed a significant difference in epithelial volume between normal and cancerous regions, however, due to limited sample size we could not demonstrate a significant difference in stromal and lumen fractional volume.Conclusion
Our study shows that HM-MRI is feasible without an endorectal coil. Fractional volumes of prostatic lumen, stroma, and epithelium in PCa can be calculated non-invasively.Acknowledgements
No acknowledgement found.References
1. Wang S, Peng Y, Medved M, et al. Hybrid multidimensional T(2) and diffusion-weighted MRI for prostate cancer detection. J Magn Reson Imaging. 2014;39:781-788.
2. Chatterjee A, Bourne RM, Wang S, et al. Diagnosis of Prostate Cancer with Noninvasive Estimation of Prostate Tissue Composition by Using Hybrid Multidimensional MR Imaging: A Feasibility Study. Radiology. 2018;287:864-873.
3. Barth BK, Cornelius A, Nanz D, Eberli D, Donati OF. Comparison of image quality and patient discomfort in prostate MRI: pelvic phased array coil vs. endorectal coil. Abdom Radiol (NY). 2016;41:2218-2226.
4. Heijmink SW, Futterer JJ, Hambrock T, et al. Prostate cancer: body-array versus endorectal coil MR imaging at 3 T--comparison of image quality, localization, and staging performance. Radiology. 2007;244:184-195.
5. Shah ZK, Elias SN, Abaza R, et al. Performance comparison of 1.5-T endorectal coil MRI with 3.0-T nonendorectal coil MRI in patients with prostate cancer. Acad Radiol. 2015;22:467-474.
6. Esses SJ, Taneja SS, Rosenkrantz AB. Imaging Facilities' Adherence to PI-RADS v2 Minimum Technical Standards for the Performance of Prostate MRI. Acad Radiol. 2018;25:188-195.
7. Costa DN, Yuan Q, Xi Y, et al. Comparison of prostate cancer detection at 3-T MRI with and without an endorectal coil: A prospective, paired-patient study. Urol Oncol. 2016;34:255 e257-255 e213.
8. Kobus T, van der Laak JA, Maas MC, et al. Contribution of Histopathologic Tissue Composition to Quantitative MR Spectroscopy and Diffusion-weighted Imaging of the Prostate. Radiology. 2016;278:801-811.
Figures
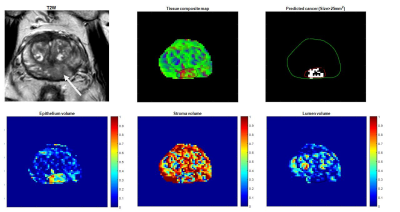
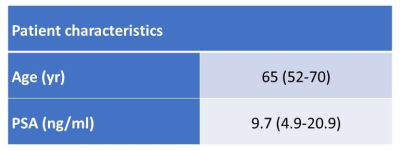
Table 1: Patient characteristics.
Means and range (within parentheses); PSA = prostate-specific antigen
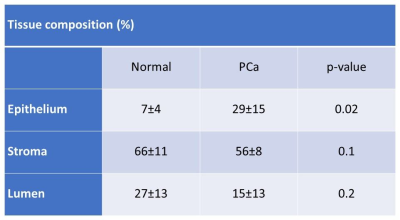
Table 2: Comparison of prostate tissue composition measured using HM-MRI.
PCa = prostate cancer