2422
Comparing multi-shot DWI with multiplexed sensitivity encoding (MUSE) with reduced field of view DWI in prostate MRI by visual grading analysis1Body MRI, Stanford University, PALO ALTO, CA, United States, 2Global MR Applications & Workflow, GE Healthcare, Waukesha, WI, United States, 3MR Body Applications & Workflow, GE Healthcare, Boston, MA, United States, 4Mathematics, Oakland University, Rochester, MI, United States
Synopsis
Diffusion-weighted imaging (DWI) using echo-planar technique is highly sensitive to susceptibility artifacts, in prostate MRI this is mainly due to rectal gas. In the hopes of identifying a sequence with better robustness to rectal gas, we compared multi-shot DWI using MUSE (with 3 shots) with a rFOV-DWI acquisition. In this IRB approved prospective study, 3 readers performed visual grading of MUSE and rFOV-DWI on 50 consecutive prostate MRI studies. MUSE-DWI and ADC maps showed statistically significant improvements in image quality for anatomic contour, lesion conspicuity, and overall image quality, as well as significantly reduced susceptibility artifacts related to rectal gas.
Synopsis
Diffusion-weighted imaging (DWI) using echo-planar technique is highly sensitive to susceptibility artifacts, in prostate MRI this is mainly due to rectal gas. In the hopes of identifying a sequence with better robustness to rectal gas, we compared multi-shot DWI using MUSE (with 3 shots) with a rFOV-DWI acquisition. In this IRB approved prospective study, 3 readers performed visual grading of MUSE and rFOV-DWI on 50 consecutive prostate MRI studies. MUSE-DWI and ADC maps showed statistically significant improvements in image quality for anatomic contour, lesion conspicuity, and overall image quality, as well as significantly reduced susceptibility artifacts related to rectal gas.Introduction
In multi-parametric prostate MRI (mpMRI), DWI is the primary sequence for evaluating malignancy in the peripheral zone of the prostate. Most implementations of DWI utilize echo-planar imaging techniques that are sensitive to susceptibility artifacts. In mpMRI, susceptibility artifacts in DWI are most commonly due to rectal gas and metal hip prosthetics. Decreasing the echo-train length can decrease the sensitivity of DWI to susceptibility artifacts. One approach is to use reduced field of view (rFOV) DWI techniques that acquire a smaller volume of tissue and consequently have a shorter echo-train. An alternative approach is multi-shot DWI techniques such as multiplexed sensitivity encoding (MUSE), where acquisition of k-space is divided into several acquisitions (“shots”). Our objective was to perform MUSE-DWI in MR prostate examinations and evaluate its efficiency in reducing artifacts compared to rFOV-DWI.Methods
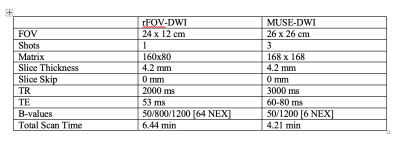
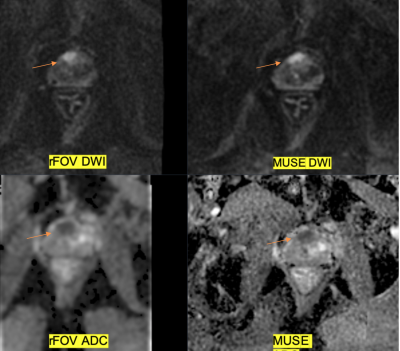
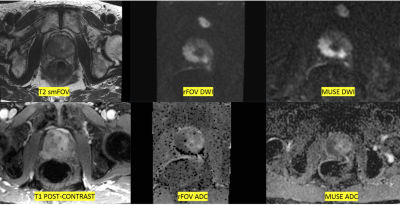
This was an IRB approved prospective trial composed of the first 50 patients undergoing 3T prostate MRI with an external 32-channel phased-array coil who consented to add the MUSE-DWI sequence. Prostatectomy patients were excluded for uniformity of grading. We compared MUSE-DWI to rFOV-DWI (GE FOCUS), scan parameters are in Table 1.Three radiologists with 10, 5, and 5 years of experience graded images. Readers were blinded to patient details, imaging sequence information, and MRI report. Images were displayed in 3 consecutive templates: 1) MUSE-DWI and ADC with axial T2 small FOV images in a 1 x 3 display pattern, 2) rFOV-DWI and ADC with axial T2 small FOV images in the same 1 x 3 format, and 3) axial T2 small FOV, axial post-contrast, MUSE-DWI and ADC, and rFOV-DWI and ADC, displayed in 2 x 3 format [Figure 2]. Whether template 1 or 2 was presented first to the reader was randomized to avoid bias.
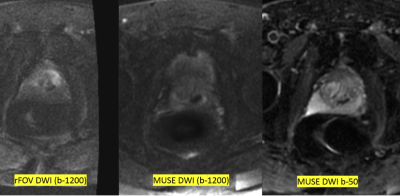
The readers graded the following on both the B-1200 DWI and ADC images for both MUSE and rFOV-DWI: the presence of artifacts (none, rectal gas, metal, other) and impact on image interpretation (yes/no), prostate contour (1-prostate margin not discerned, 2-margin discernible but peripheral/transitional zone, not well-demarcated, 3-prostate margin and peripheral/transitional zone demarcation sharp), lesion presence and conspicuity (0-no lesion, 1-lesion faintly visualized, 2-lesion seen with blurry margins, 3-lesion with sharp margins). Relative grading was performed during side-by-side visualization of the B-1200 DWI and ADC images for both MUSE and rFOV-DWI (0-similar image quality in both methods, +1 MUSE better, -1 rFOV-DWI better).
Wilcoxon ranked sum test and McNemar tests were used for statistical analysis. Significance was set to a p-value of < 0.05, with a Holm-Bonferroni correction used due to multiple comparisons. Interobserver variability was calculated using Cohen’s kappa analysis.
Results
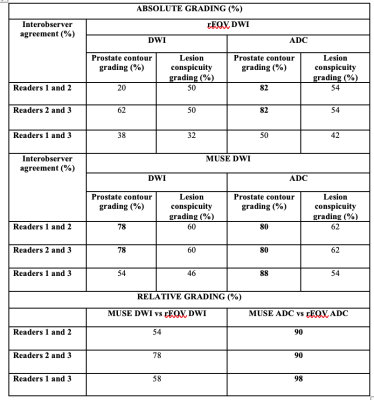
Radiology reports demonstrated no lesion in 30.6% of studies, with the reminder having a dominant lesion assessed as PI-RADS 3 (8%), PI-RADS 4 (34.7%), or PI-RADS 5 (26.5%). There was a statistically significant difference with fewer limiting artifacts reported with MUSE-DWI and ADC over rFOV (MUSE 32% of reads with artifacts of which only 31.2% limited evaluation versus rFOV-DWI with artifact in 36% of reads of which 94.4% limited evaluation, p=.001).The interobserver variability on the absolute visual grading parameters shows that there was higher interobserver agreement with MUSE images and also between readers 2 and 3 [Table 2]. The quantitative ADC values of the dominant lesion were predominantly lower in MUSE (mean 880.6; median 853.5) compared to rFOV-DWI (mean 963.9; median 919.0), although this was not statistically significant (two-sample T-test p=0.079). The reason for this trend toward differences in ADC values may stem from incorporation of an additional B-800 DWI acquisition in the rFOV-DWI acquisition, this B-800 information was incorporated into the resultant rFOV-ADC calculation.
Discussion
We noticed a significantly reduced rate of susceptibility artifact limiting prostate evaluation with MUSE compared to rFOV-DWI. This reduction in susceptibility artifact may stem from the shorter echo train of MUSE (56 for the case of 3 shots in our study) versus rFOV-DWI. This indicates further robustness from susceptibility artifact could be made from further reducing the echo train by using a greater number of shots or utilizing acceleration. There was a consistent and significant interobserver agreement between the readers for the MUSE ADC images to be higher image quality.Conclusion
By visual grading analysis, MUSE-DWI was significantly preferred compared to rFOV-DWI and demonstrated better delineation of prostate margin and lesion conspicuity on MUSE-DWI. MUSE also demonstrated significantly less susceptibility artifacts due to rectal gas. In conclusion, compared to rFOV-DWI, MUSE-DWI demonstrates potential improvements for prostate MRI due to increased robustness to the effects of rectal gas and improvements in image quality.Acknowledgements
No acknowledgement found.References
1. Chen NK, Guidon A, Chang HC, Song AW. A robust multi-shot scan strategy for high-resolution diffusion-weighted MRI enabled by multiplexed sensitivity-encoding (MUSE). NeuroImage 72 (2013), 41-47.
2. Guhaniyogi S, Chu ML, Chang HC, Song AW, Chen NK. Motion Immune diffusion imaging using augmented MUSE for high-resolution multi-shot EPI. Magnetic Resonance in Medicine 75 (2016):639-652.
3. Bruce IP, Chang HC, Petty C, Chen NK, Song AW. 3D-MB-MUSE: A robust 3D multi-slab, multi-band and multi-shot reconstruction approach for ultrahigh-resolution diffusion MRI. NeuroImage 159 (2017):46-56.
4. Precht H, Hansson J, Outzen C, Hogg P, Tingberg A. Radiographers’ perspectives’ on Visual Grading Analysis as a scientific method to evaluate image quality. Radiography 25 (2019): S14-S18.
Figures