2420
Does intramuscular injection of glucagon improve prostate MR image quality?1Radiology, Stanford University School of Medicine, Stanford, CA, United States, 2Department of Radiology, Veterans Affair Palo Alto Healthcare System, Palo Alto, CA, United States
Synopsis
ACR PI-RADs guidelines suggest anti-spasmodic agents may be beneficial for some patients during multi-parametric prostate MRI (mpMRI). Recent evidence suggests that the anti-spasmodic scopolamine butylbromide improves image quality on mpMRI. However, no studies have evaluated intramuscular (IM) injected glucagon. This retrospective IRB approved single-center study performed data-mining of 2595 mpMRI radiology reports (693 with glucagon) and subjective image quality assessment of 63 mpMRI exams (32 with glucagon). No significant benefit of IM glucagon for prostate evaluation was found on mpMRI. Our findings suggest that the risks associated with IM glucagon (medication side effects, patient discomfort, cost) may outweigh any benefits.
Introduction
Anti-spasmodic agents are often used in abdominal MRI to limit motion of bowel during exams that target adjacent organs. The new version of PI-RADs (v2.1, 2019) suggests that anti-spasmodic agents (e.g. glucagon, scopolamine butylbromide, or sublingual hyoscyamine sulfate) may be beneficial in some patients1. Recent evidence suggests improved image quality and reduced motion-related artifacts in multi-parametric prostate MRI (mpMRI) after IV injection of scopolamine butylbromide2,3, an anti-cholinergic with high affinity for muscarinic receptors in colonic and bowel smooth muscle4. Since scopolamine butylbromide is not available in the U.S, many centers instead use intramuscular (IM) administration of glucagon, a peptide acting on G-protein coupled receptors5. However, there are no published studies evaluating the effect of IM glucagon on mpMRI image quality. We evaluated MR image quality from patients undergoing mpMRI after the IM administration glucagon compared to those who did not receive glucagon.Methods
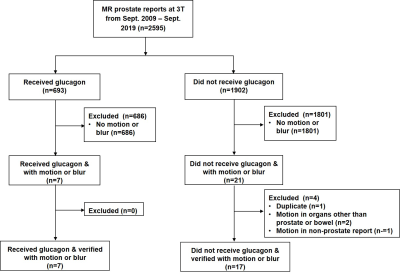
This retrospective observational study was approved by our institutional review board and took advantage of an institutional change in protocol to discontinue the use of glucagon (1 mg IM) in patients undergoing mpMRI. This study expands upon a previous abstract6 by using a larger number of cases, a larger number of readers, and includes a data mining approach. All mpMRI examinations were performed on 3.0 Tesla scanners (GE MR750, Waukeshaw Wisconsin, USA) utilizing external 32-channel phased array coils. Imaging parameters for the small field-of-view T2-weighted image sequence were: Fast spin-echo, 416 x 224 matrix, 3.6-mm slices, NEX 2, 20-cm FOV, TE 130 ms, TR 4100 ms. Scan time: 2.04 min.Data mining of radiology reports was performed using Montage™, a radiology report data-mining system that finds reports containing specific keywords and derivations. We examined 2595 MRI prostate reports from our institution performed between September 2009 and September 2019 and searched for the keywords “motion” or “blur”.
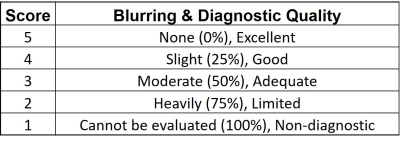
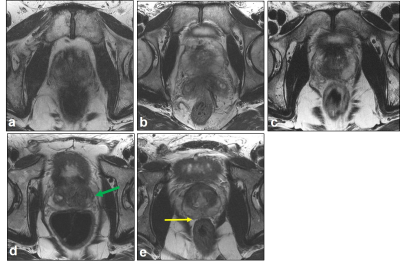
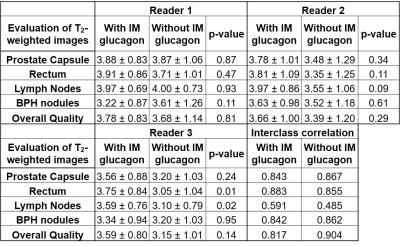
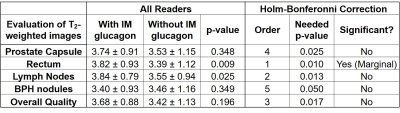
Qualitative assessment of image quality was performed using 3 radiologists with 10, 8, and 5 years of experience interpreting prostate MRI studies. Readers were blinded to patient identity, study date, and administration of IM glucagon. Readers independently scored 64 cases (a series of cases within a 5-month period, 32 sequentially before and 32 sequentially after discontinuation of glucagon) for motion-related blurring of pelvic organs. One case without IM glucagon was excluded from analysis due to the presence of brachytherapy seeds. The prostate capsule, rectum, lymph nodes, benign prostatic hyperplasia (BPH) nodules, and overall image quality on small field-of-view T2-weighted sequences were scored using a 5-point Likert scale (Table 1). Reference training set images were provided to the readers (Figure 1). Readers scrolled through the full stack of images.
The null hypothesis of no significant difference in scores was assessed using a Mann-Whitney U Test for two independent samples (a = 0.05). An interclass correlation coefficient (a = 0.05) was used to evaluate for inter-observer agreement among the 3 readers7. To correct for familywise error rates, a Holm-Bonferroni Method correction was applied.
Results
Examination of 2595 MR prostate reports over a 10 year period demonstrates that only 1.01% (7/693) mentioned “blur” or “motion” in patients administered IM glucagon while 0.89% (17/1902) mentioned “blur” or “motion” in patients who did not receive IM glucagon (Figure 2). Qualitative assessment of 63 cases by 3 readers demonstrated no effect of glucagon in the evaluation of the prostate capsule, lymph nodes, BPH nodules, and overall image quality on T2-weighted images. However, significant differences were observed in evaluation of the rectum, where blurring appeared improved after administration of IM glucagon (3.74 vs 3.52, p=0.009, Tables 2 and 3). Intra-class correlation coefficient analysis revealed good reliability between readers when measuring prostate capsule, rectum, BPH nodules, and overall image quality8. Borderline moderate reliability between readers was observed for scoring of lymph nodes (Table 3)8.Discussion
Our retrospective data-mining review shows that glucagon did not change the percentage of prostate MRIs where radiologists mentioned “blur” or “motion,” suggesting IM glucagon does not improve the quality of mpMRI. Our assessment found a small but significant effect of glucagon on decreasing rectal wall motion, which is consistent with the expected and intended effect of the medication. However, we found no significant differences in evaluation of the prostate capsule boundary, BPH nodules, lymph nodes, and overall image quality of mpMRI. This suggests that IM glucagon may have a minor but detectable effect on the organ targeted by the medication (rectum) but does not impact overall image quality for the primary organ of interest in the exam (prostate). One limitation of our study is the inability to reliably distinguish bowel motion from bulk patient motion or other artifacts. However, our study suggests that the marginal benefit of IM glucagon for mpMRI is outweighed by potential adverse effects of the medication, patient discomfort, and additional time and cost.Conclusion
Although a marginally significant difference in rectal wall motion was observed with administration of IM glucagon, we found no detectable difference in evaluation of other pelvic organs or overall image quality with administration of IM glucagon for mpMRI of the prostate at 3T. Future larger prospective studies may explore the use of IV or IM glucagon or sublingual hyoscyamine sulfate on blurring and diagnostic quality of mpMRI.Acknowledgements
We would like to thank the body MRI faculty and fellows for input during weekly discussions.
References
1. Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76(3):340-351.
2. Slough RA, Caglic I, Hansen NL, Patterson AJ, Barrett T. Effect of hyoscine butylbromide on prostate multiparametric MRI anatomical and functional image quality. Clin Radiol. 2018;73(2):216.e9-216.e14.
3. Ullrich T, Quentin M, Schmaltz AK, et al. Hyoscine butylbromide significantly decreases motion artefacts and allows better delineation of anatomic structures in mp-MRI of the prostate. Eur Radiol. 2018;28(1):17-23.
4. Tytgat GN. Hyoscine butylbromide: A review of its use in the treatment of abdominal cramping and pain. Drugs. 2007;67(9):1343-1357.
5. Mayo KE, Miller LJ, Bataille D, et al. International Union of Pharmacology. XXXV. The glucagon receptor family. Pharmacol Rev. 2003;55(1):167-194.
6. Chang ST, Vasanawala SS, Loening AM. Does Intramuscular Glucagon for Prostate MRI Improve Image Quality? 2016 International Society for Magnetic Resonance in Medicine (ISMRM). May 7-13. Singapore (Abstract #1596).
7. Hallgren KA. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor Quant Methods Psychol. 2012;8(1):23-34.
8. Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155-163.
Figures