2415
RADIOLOGICAL COURSE OF SUB-CENTIMETER ARTERIALLY ENHANCING NODULES DETECTED DURING SURVEILLANCE FOR HEPATOCELLULAR CARCINOMA1Medanta Hospital, Gurgaon, India, 2Medanta Hospital, GURGAON, India
Synopsis
Clinical data on the course of sub-centimeter-sized nodules (SCSNs) detected during surveillance for HCC is limited. Through this study we wished to evaluate arterially enhancing SCSN evolving into HCC. We tried identify specific size cut off, rate of growth, enhancement features which can predict which SCSN will turn into HCC. 47.5% of SCSN have the potential to turn into HCC. 8.55 mm is the optimal size cut off above which risk of developing HCC increases with a sensitivity of 71.4%. Diffusion restriction was seen in 50% and non uptake of hepatobiliary contrast in 91% of SCSN which developed into HCC.
INTRODUCTION
HCC detection at an early stage can allow for timely implementation of effective treatment strategies and improve survival. Presently a wait and watch policy is recommended for nodules smaller than 1 cm. However, there is a high possibility that minute arterially enhancing hepatic nodules detected during surveillance may become malignant over time. Nevertheless, clinicians have limited data on the radiological course of sub-centimeter-sized arterially enhancing nodules (SCSNs) detected during surveillance.Through this study we wished to evaluate the outcome and incidence of arterially enhancing subcentimeter nodules evolving into HCC. Further to identify specific radiological MRI features which can prognosticate and if possible predict which SCSNs will turn into HCC.
METHODS
We prospectively analyzed a total of 60 patients with liver cirrhosis or chronic hepatitis B or C without a prior history of HCC in whom a SCSN was detected during HCC surveillance. The patients were followed for a period of two years but any previous imaging if available was also included in the analysis. The imaging was done on Siemens Magnetom Verio 3 Tesla and Siemens Magnetom Aera 1.5 Tesla. Dynamic MRI scans performed were in accordance with the protocol recommended by American College of Radiology (practise parameter for MRI of liver Res. 3 - 2015). Dynamic Post Contrast MRI was acquired following 0.1 mmol/kg of Multihance. Delayed hepatobiliary phase imaging was also acquired.Following imaging characteristics of the lesion were taken into account. (1) Signal intensity T2 / T1 Hyper / Iso / Hypointense, (2) Diffusion restriction, (3) Arterial enhancement, (4) any wash out, (5) rim enhancement, (6) size and (7) non-uptake of hepataobiliary contrast.
The gold standard for HCC diagnosis was an LR 5 lesion (LIRADS version 2018) reached in consensus with two expert abdominal radiologists. We calculated the rate of HCC development from SCSNs in the study population and analyzed the differences in imaging features between the patients with SCSNs that eventually developed into HCC and patients with SCSNs that did not develop into HCC. Student t test was used for comparison of quantitative outcome parameters. Area under the curve was calculated using ROC curve analysis. The cut off values along with corresponding sensitivity & specificity were also calculated.
RESULTS
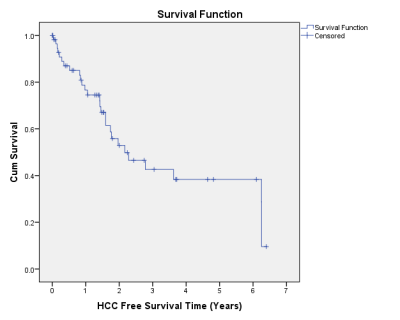
60 patients were scanned over mean duration of 4.5 years ( range 3-6.5 years). The cumulative HCC development rate was 47.5%. Upon baseline comparison, the growth difference was more in the HCC group (8.13±12.24mm) in comparison to the non HCC group (3.37±7.39 mm) during the imaging interval. 60.9% of the HCC lesions showed an increase in size, 31.6% of the non HCC lesions also showed an increase in size. The optimal cut off points after which the likelihood of an arterially enhancing lesion turning into HCC was 8.5mm with a sensitivity of 72.7 % and a specificity of 66.7%. For subcentimetric arterially enhancing nodules the mean HCC free interval was 3.3years. At a time interval of 1 year 59.7% of the lesions did not change into HCC and at an interval of 4 years 45.2% of the lesions did not convert into malignancy. All the patients in the HCC group showed washout and 91% showed non-uptake of hepatobiliary contrast. Diffusion restriction was seen in 50% while rim enhancement in 33% of patients in the HCC group. As expected T1 and T2 signal intensities were not significant indicators of HCC development.DISCUSSION AND CONCLUSION
Around 47.5% of SCSN have the potential to turn into HCC, this is a higher rate compared to published literature. At a time interval of 1 year 59.7% of the lesions did not change into HCC. Hence the optimal time for following up of the patient should be every 6 months-upto 40% of lesions might turn into HCC in a span of less than one year. Also it is possible for lesions to convert into HCC even after remaining stable for 3-4 years, therefore, hypervascular lesions should be followed up for at least 6 years. Diffusion-weighted imaging may improve the diagnostic performance of MRI for small HCCs by demonstrating higher cellularity of HCC. In our study 50% of HCCs gave diffusion restriction. Hence, not all HCC lesions demonstrated diffusion restriction on MRI. Hepatobiliary phase hypointensity is a strong predictor of premalignancy or malignancy, In our study out of all who developed HCC 91% of patients showed non-uptake of hepatobiliary contrast.This study can be used to power other large multicentric trials with larger sample sizes to further develop recommendations for sub-cm arterially enhancing nodules in HCC surveillance.
Acknowledgements
No acknowledgement found.References
1.American College of Radiology. ACR–SAR–SPR Practice Parameter for the Performance of Magnetic Resonance Imaging (MRI) of the Liver Res. 3 - 2015. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/MR-Liver.pdf. Accessed April 3, 2017.
2. American College of Radiology: Liver Imaging Reporting and Data System. https://nrdr.acr.org/lirads/. 2018. Accessed September 3, 2018
3. Choi BI, Lee JM, Kim TK, Burgio MD, Vilgrain V. Diagnosing Borderline Hepatic Nodules in Hepatocarcinogenesis: Imaging Performance. Am J Roentgenol. 2015; 205(1):10–21.
4. Chou C-T. Differentiation between dysplastic nodule and early-stage hepatocellular carcinoma: The utility of conventional MR imaging. World J Gastroenterol. 2013;19(42):33-47.
5. Min YW. Clinical course of sub-centimeter-sized nodules detected during surveillance for hepatocellular carcinoma. World J Gastroenterol. 2012;18(21):26-54.