2395
High Resolution Prostate T2-weighted MRI with Deep Learning and without an Endorectal Coil1Global MR Applications & Workflow, GE Healthcare, Houston, TX, United States, 2Department of Imaging Physics, MD Anderson Cancer Center, Houston, TX, United States, 3Department of Abdominal Imaging, MD Anderson Cancer Center, Houston, TX, United States, 4Department of Cancer Systems Imaging, MD Anderson Cancer Center, Houston, TX, United States, 5Global MR Applications & Workflow, GE Healthcare, Calgary, AB, Canada
Synopsis
Endorectal coil (ERC) offers high SNR that is needed for high-resolution prostate MRI, which is essential for accurate visualization of prostate and detection of prostate cancer. Unfortunately, use of an ERC is cumbersome, costly, and discomforting or even intolerable to some patients. Further, ERC often has exacerbated motion artifacts due to its proximity to the regions of interests. In this work, we applied a novel deep learning-based MR reconstruction method to clinical prostate T2-weighted imaging without an ERC (non-ERC). DL Recon improved non-ERC image SNR, reduced artifacts, and improved overall image quality compared to conventional reconstruction with/without endorectal coil.
Introduction
Endorectal coil (ERC) offers high SNR that is needed for high-resolution prostate MRI1,2, which is essential for accurate visualization of prostate and its surrounding anatomy and detection of prostate cancer. Unfortunately, use of an ERC is cumbersome, costly, and discomforting or even intolerable to some patients3. Further, ERC often has exacerbated motion artifacts4 due to its proximity to the regions of interests. In this work, we applied a novel deep learning-based MR reconstruction method (hereby named “DL Recon”) to clinical prostate T2-weighted (T2W) imaging without an ERC (non-ERC). To evaluate its performance in boosting SNR and mitigating artifacts, we compared the non-ERC images reconstructed with DL Recon with the images reconstructed with conventional reconstruction with and without ERC.Materials and Methods
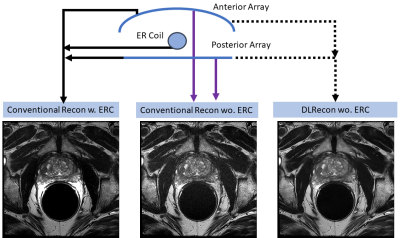
20 patients who underwent clinical prostate MRI exams were included in this IRB-approved study. Raw data from high-resolution T2W images (FOV=16cm, matrix=256x256, 3mm slices) were acquired with an ERC in combination with a phased array coil on GE 1.5T 450w (9 cases) and GE 3T MR750w (11 cases) scanners (Waukesha, WI). The DL Recon comprised a deep convolutional residual encoder network trained using a prior database. The network offered a tunable noise reduction factor to accommodate user preference, which was selected as 75% in this study. In addition to the conventional standard reconstruction using both ERC and phased array coils, two sets of images were generated by DL Recon and conventional recon after excluding the signal from ERC (Fig. 1). These images were blindly reviewed and scored qualitatively by three experienced radiologists using a 5-point Likert-scale for key image quality metrics and artifacts. Each radiologist scored the visualization of the prostate capsule, neurovascular bundle, anterior rectal wall and the visualization of the central and peripheral zones of the prostate. The overall image artifacts and overall image quality were also evaluated. The scores were compared using Tukey’s multiple comparisons test. GraphPad Prism 8 (GraphPad, San Diego, Calif) was used to perform the statistical analyses, with P < .05 considered to be statistically significant.Results
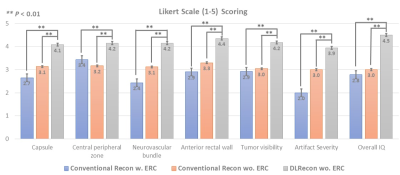
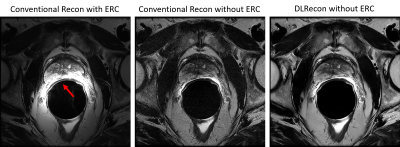
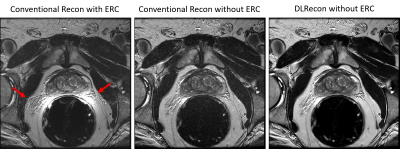
Images by DL Recon without ERC were scored consistently higher in all categories compared to the conventional recon (with or without ERC) (Fig. 2). Compared to the images by the conventional recon (with or without ERC), DL Recon images showed improved visualization in prostate capsules (4.1 vs 2.7, 3.1, P<0.01), central glands (4.2 vs 3.4, 3.2, P<0.01), neurovascular bundles (4.2 vs 2.4, 3.1, P<0.01), anterior rectal wall (4.4 vs 2.9, 3.3, P<0.01), and tumors (4.2 vs 2.9, 3.0, P<0.01). Artifacts are also less severe in DL Recon images without ERC (4.0 vs 2.2, 3.1, P<0.01). The images by conventional recon without ERC scored higher than with ERC in most categories, except in the definition of the central gland (CG) vs. peripheral zone (PZ). Since approximately 70% of prostate cancer is found in PZ, the use of ERC is understandably important. However, DL Recon significantly improved the image quality and even scored higher than conventional recon with ERC in the definition of CG vs. PZ. Images by conventional recon with ERC had the most artifacts with large signal intensity inhomogeneities (Fig. 3, red arrow). ERC may also produce enhanced motion artifacts (Fig. 4, red arrow) with conventional reconstruction. Removing signal from ERC with conventional recon can reduce the intensity inhomogeneities and motion artifacts but result in reduced SNR. However, DL Recon improved the SNR of the images reconstructed without ERC as well as reducing intensity inhomogeneities and motion artifacts.Conclusion and Discussion
DL Recon provided high quality prostate T2W MR imaging without an ERC. The direct and qualitative comparison by 3 experienced radiologists showed that the overall quality of the DL Recon images without an ERC is significantly better than that of conventional recon with or without ERC. DL Recon images showed improved visualization of prostate capsules, CG, neurovascular bundles, anterior rectal wall and tumors.Acknowledgements
No acknowledgement found.References
1. Fütterer, JJ, Scheenen T, Huisman H, et al. Initial experience of 3 tesla endorectal coil magnetic resonance imaging and 1H-spectroscopic imaging of the prostate. Investigative Radiology. 2004;39(11): 671-680.
2. Bloch, B. N., Rofsky, N. M., Baroni, R. H, et al. 3 Tesla magnetic resonance imaging of the prostate with combined pelvic phased-array and endorectal coils: Initial experience. Academic radiology. 2004;11(8):863-867.
3. Barth, B. K., Cornelius, A., Nanz, D., et al. Comparison of image quality and patient discomfort in prostate MRI: pelvic phased array coil vs. endorectal coil. Abdominal Radiology. 2016;41(11):2218-2226.
4. Noworolski, S. M., Crane, J. C., Vigneron, D. B., & Kurhanewicz, J. A clinical comparison of rigid and inflatable endorectal‐coil probes for MRI and 3D MR spectroscopic imaging (MRSI) of the prostate. J. Magn. Reson. Imaging. 2008;27(5):1077-1082.
Figures