2372
Assessing void artifacts in follow-up breast MRI scans after sentinel node biopsy using superparamagnetic tracer1Techmed Centre, University of Twente, Enschede, Netherlands, 2Department of Radiology, Medisch Spectrum Twente, Enschede, Netherlands, 3Department of Surgery, Medisch Spectrum Twente, Enschede, Netherlands
Synopsis
Sentinel lymph node biopsy using a magnetometer and a superparamagnetic iron oxide (SPIO) tracer is currently being introduced for breast cancer patients eligible for breast conserving surgery. However, the residual SPIOs potentially result in void artifacts in follow-up MRI examinations. This study assesses the influence of injection dose on the severity of the void artifacts in follow-up MRI by means of qualitative grading by radiologists.
Introduction
Sentinel lymph node (SLN) biopsy using a radioisotope tracer (99mTc-nanocolloid) alone, or combined with a blue dye, is the world-wide standard of care for axillary staging of early-stage breast cancer patients. To avoid radiation-associated issues, a handheld magnetometer was developed for intraoperative SLN identification1. This magnetometer utilizes the magnetic signal produced by an interstitially administered superparamagnetic iron oxide (SPIO) tracer. However, after breast conserving surgery, residual SPIO tracer potentially results in void artifacts in follow-up MRI examinations2,3. This study investigates the influence of injection dose on the severity of void artifacts in follow-up MRI by means of qualitative grading.Methods
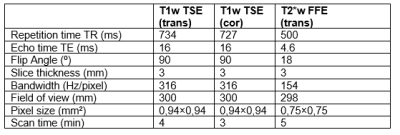
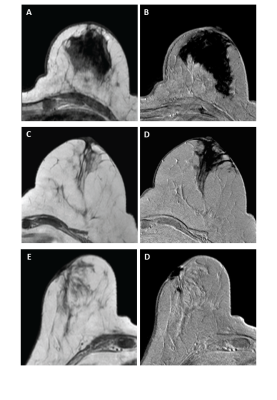
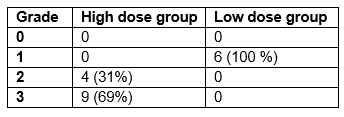
All patients referred for breast cancer surgery with axillary lymph node staging received SLN biopsy (SLNB) using a radioactive tracer 99mTc and Patent Blue dye. In the period between May 2012 and March 2015, 76 patients were included in the SentiMAG multicentre trial4 and MagSNOLL trial5 in which additional superparamagnetic tracer (Sienna+®, Sysmex Europe, Hamburg, Germany) was injected into the breast. In the SentiMAG study the patients received a sub-areolar injection of 2mL of SPIO particles diluted in 3 ml saline (high dose group), while in the MagSNOLL study the patients were injected intra-tumorally with 0.1mL SPIO particles (low dose group). This 0.1mL was defined as the lowest dose that still enabled sentinel lymph node identification intraoperatively. All patients were scheduled for a SLNB with clinically and radiologically negative SLN. Pregnant women, patients with known intolerance or hypersensitivity to iron or dextran compounds, and patients with pacemakers or other implantable devices on the chest wall were excluded. Of the 76 patients invited for a follow-up MRI, 41 patients had a mastectomy, 5 were lost to follow-up due to death, and 11 patients refused to participate. Consequently, 19 patients were included in a follow-up breast MRI study: 13 participants in the high dose group and 6 in the low dose group. Data was acquired with a 1.5T MR system (Intera, Philips Medical Systems, Best, the Netherlands) using a dedicated breast coil. T1-weighted (T1w) turbo spin echo (TSE) MRI was acquired in the transverse and coronal plane, while T2*-weighted (T2*w) gradient echo (GRE) MRI was acquired only in the transverse plane. Table 1 summarizes the acquisition parameters. All MRI scans were analyzed using DynaCAD® workstation (Philips Healthcare, Best, the Netherlands). The analysis was with respect to susceptibility artifacts due to SPIO remnants by consensus of two radiologists with years of experience in breast imaging. On the transverse T1w and T2w MRI, grading of void artifacts was performed using a four-point scale. Grade 0 defines there is no artifact visible, grade 1 defines a minimal artifact with diagnostic evaluation possible, grade 2 defines moderate artifacts with impaired diagnostic evaluation, grade 3 defines severe artifacts in the image.Results
The follow-up MRI after SLNB was acquired within four years in the high dose group (mean 2.9 years, range 2.5-3.4 years), and within one year in the low dose group (mean 0.6 years, range 0.5-0.7 years). Typical examples of the void artifacts of different grades can be seen in Figure 1. Especially in the case of the grade 3 artifact large signal gaps in the breast are present, severely hampering follow-up diagnosis. The results of the qualitative grading of all patients can be seen in Table 2. There is a distinct difference between both groups, with the low dose group having only grade 1 artifacts whereas in the high dose group all images at least had impaired diagnostic evaluation (minimal grade 2, mean grade 2.7).Discussion
Subareolar administration of superparamagnetic tracer at a high dose (2 mL tracer in 3 mL saline) in patients undergoing breast conserving surgery resulted in more residual SPIO particles in the majority of patients, leading to a high grade of artifacts. This hinders the interpretation of follow-up MRI scans up to 3.6 years after the SLNB. Both injections were done in two separate sites (sub-areolar and intra-tumoral) making a full direct comparison impossible. However, the lowered dose clearly has an advantage in decreasing the void artifacts, and by this new insight it seems better to place the tracer within the tissue of the resection.Conclusion
The void artifacts on follow-up MR imaging can be largely prevented by using a low dose (0.1 mL) intra-tumoral administration of SPIOs for SLN detection. This results in possible diagnostic evaluation of all follow-up scans in this group of patients.Acknowledgements
The authors would like to acknowledge Muneer Ahmed and Michael Douek for their valuable feedback.References
1.Ahmed, M., Purushotham, A. D.
& Douek, M. Novel techniques for sentinel lymph node biopsy in breast
cancer: a systematic review. Lancet Oncol
15, e351-362,
doi:10.1016/S1470-2045(13)70590-4 (2014).
2. Forte, S.,
Kubik-Huch, R. A. & Leo, C. Improvement in breast magnetic resonance
imaging after a sentinel procedure for breast cancer with superparamagnetic
tracers. Eur J Radiol Open 6, 215-219,
doi:10.1016/j.ejro.2019.05.006 (2019).
3. Krischer, B.,
Forte, S., Niemann, T., Kubik-Huch, R. A. & Leo, C. Feasibility of breast
MRI after sentinel procedure for breast cancer with superparamagnetic tracers. Eur J Surg Oncol 44, 74-79, doi:10.1016/j.ejso.2017.11.016 (2018).
4. Thill, M. et al. The Central-European SentiMag
study: sentinel lymph node biopsy with superparamagnetic iron oxide (SPIO) vs.
radioisotope. Breast 23, 175-179, doi:10.1016/j.breast.2014.01.004 (2014).
5. Ahmed, M. et al. Magnetic sentinel node and
occult lesion localization in breast cancer (MagSNOLL Trial). Br J Surg 102, 646-652, doi:10.1002/bjs.9800 (2015).
Figures