2367
Phase imaging of hyperpolarized 129Xe gas in a human lung1Monash Biomedical Imaging, Monash University, Clayton, Australia, 2Australian Nuclear Science and Technology Organisation, Lucas Heights, Australia, 3Instrument Technologies Division, European Spallation Source ERIC, Lund, Sweden, 4China Spallation Neutron Source, Dongguan, China, 5Delft University of Technical, Delft, Netherlands, 6Eastern Clinical School, Monash University, Box Hill, Australia
Synopsis
We describe a custom-designed spin-exchange-optical pumping (SEOP) polarizer which can reliably produce hyperpolarized 129-Xe (HP-Xe) gas. Imaging of a HP-Xe phantom showed phase images were less sensitive to depolarization and could provide on/off images of HP-Xe. In a human lung, phase image provided higher imaging contrast in low HP-Xe polarization states.
Introduction
HP-Xe can be rapidly depolarized by oxygen and radiofrequency (RF) pulses during magnetic resonance (MR) imaging in lung1,2. When HP-Xe flows into the lung, the distances of gas path are different in different regions which could cause different depolarization of HP-Xe. It is difficult to distinguish the signal loss on routine magnitude images is related with disease or caused by depolarization. The aim of this study was to use the phase image to image HP-Xe in a human lung.Materials and methods
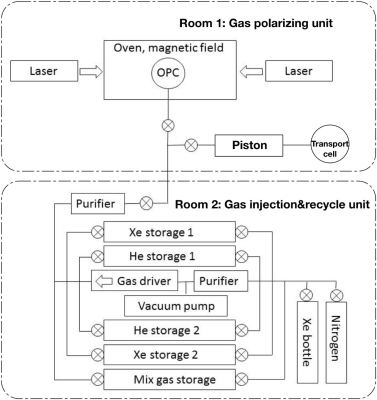
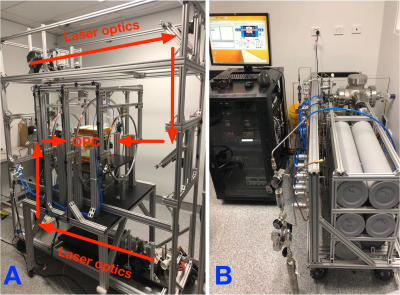
129Xe gas is polarized by a customized spin-exchange-optical pumping (SEOP) polarizer by batches rather than a continuous-flow process. Its diagram is shown in Figure 1. The polarizer consists of a gas-polarizing unit and a gas injection/recycle unit. To reduce the interactions, the two units were placed in two different rooms (See Figure 2). The gas-injection circuit sequentially flows Xenon and nitrogen into the OPC and the ratio between them is 1:4. After polarizing for 30-40 minutes, the gas is transferred from OPC to the transport cell by a piston and immediately taken into MRI room.All MR experiments were performed on a Siemens 3T scanner (Skyra, Siemens Medical Solutions, Erlangen, Germany) with a bird-cage 129Xe lung coil (RAPID Biomedical GmbH, Wuerzburg, Germany). The resonance frequency of 129Xe was set to 34.09 MHz. A 2D-GRE sequence was used for 129Xe gas imaging. For phantom imaging, the parameters were as follows: flip angle = 7o, repetition time = 15 ms, echo time = 3.24 ms, field of view = 400*400 mm2, matrix size = 96*96, single slice, slice thickness = 25 mm, bandwidth = 370 Hz/Pixel, 4 averages and 4 repetitions. For human lung imaging, the parameters were flip angle = 7o, repetition time = 20 ms, echo time = 7.81 ms, field of view = 500*500 mm2, matrix size = 64*64, single slice, slice thickness = 180 mm, bandwidth = 50 Hz/Pixel, and 6 averages.
Results and discussions
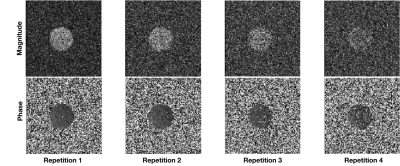
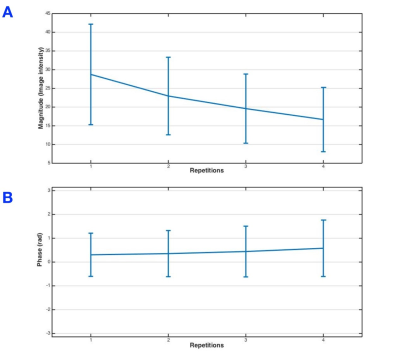
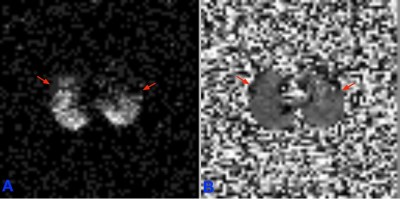
Figure 3 shows the changes in the magnitude (Figure 3 first row) and phase (Figure 3 second row) images in a 129Xe gas phantom. Figure 4 demonstrates the corresponding image intensity and variance of the magnitude and phase images. The image intensities of the magnitude images decreased following each repetition, while that of phase images was nearly unchanged, supporting that the phase images were less affected by depolarization induced by the RF excitation.Figure 5 shows the magnitude and phase images of a human lung in the axial plane. There was an increasing signal intensity in the magnitude image from anterior to posterior (Figure 5A), which might associate with gravity-dependent gradient in the human lung tissue density from anterior to posterior in the supine position3. However, there was no such a change in the phase image (Figure 5B). The phase image was computed by the arctangent of the ratio between the real and imaginary parts. Since the real and imaginary signals originate from the same source, they have similar signal and noise distributions which might effectively cancel both the gradient and the noise. Because of such a cancellation, the phase image can work in on/off mode to show HP-Xe in a low concentration.
The signal loss in the anterior part of lung in the magnitude image (red arrows in Figure 5A) could be also caused by the depolarization of HP-Xe. Phase image has the capability in imaging low-level HP-Xe in the anterior part of lung (red arrows in Figure 5B).
Conclusions
Phase image is less sensitive to the depolarization, and can work in on/off mode to show whether or not there is HP-Xe in lung. Measuring the phase signal has the potential for improved sensitivity for HP-Xe imaging.Acknowledgements
We would like to acknowledge the supports of the Australian Research Council (Grant LE130100035), the National Health and Medical Research Council (Grant APP606944), and CASS foundation for the polarizer and the Australian National Imaging Facility Fellowship.References
[1] Dregely I, Ruset IC, Wiggins G, Mareyam A, Mugler JP 3rd, Altes TA, Meyer C, Ruppert K, Wald LL, Hersman FW. 32-channel phased-array receive with asymmetric birdcage transmit coil for hyperpolarized xenon-129 lung imaging. Magn Reson Med. 2013; 70(2):576–583.1
[2] Doganay O, Matin TN, Mcintyre A, Burns B, Schulte RF, Gleeson FV, Bulte D. Fast dynamic ventilation MRI of hyperpolarized 129 Xe using spiral imaging. Magn Reson Med. 2018 May;79(5):2597-2606.
[3] Mugler JP, Altes TA. Hyperpolarized 129Xe MRI of the human lung. J Magn Reson Imaging. 2013; 37(2):313–331.
Figures