2361
Pulmonary nodule detection using ultra-short TE (UTE) with a 3D variable-TE stack-of-spirals sequence in a 3T MR-PET scanner1Department of Medical Imaging, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan, 2Department of Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan
Synopsis
Although the 3T MR-PET system has been used clinically for the whole body, PET/CT still has advantages over this technique when evaluating the pulmonary region. Ultrashort TE with 3D variable-TE stack-of-spirals sampling has been used for pulmonary nodule detection in MR examination1, which allows for shorter scanning times using an undersampling technique in combination with iterative self-consistent parallel imaging reconstruction (SPIRiT). The goal of this study was to investigate the feasibility of this technique for detecting pulmonary nodules in the 3T MR-PET scanner, which has fewer coil elements compared with most other MR-only scanners, to achieve minimum PET attenuation.
Introduction
MRI and PET systems are advantageous for imaging2,3, but image quality for the lung is problematic for MR-PET. Considering a short T2 and T2* value in the lung, the 3D variable-TE ultrashort TE stack-of-spirals VIBE sequence4,5 (spiral UTE VIBE) is proposed for lung MRI. This sequence has spiral integrated parallel acquisition with the image reconstruction performed by iterative self-consistent parallel imaging reconstruction (SPIRiT) from the arbitrary k-space technique6-7. In this study, the spiral UTE VIBE sequence was used for a 3T MR-PET scanner that had fewer coil elements for the minimum PET attenuation compared with our previous study with a 1.5T MR scanner. We aimed to first assess the spiral UTE VIBE image quality in a 3T MR-PET scanner with fewer coil elements, and second, to detect lung nodules using the spiral UTE VIBE sequence in the 3T MR-PET scanner and investigate the agreement of the nodule sizes, comparing them with CT images.Methods
The hospital’s Institutional Review Board approved this study, and informed consent was obtained from all enrolled subjects. Images were acquired on a 1.5T scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) and 3T MR-PET scanner (Biograph mMR, Siemens Healthcare, Erlangen, Germany). Subjects enrolled for the 3T scanner were all health-check customers, whereas those with a known lung nodule were scheduled for lung wedge resection and enrolled for the 1.5T scanner. The patient demographic information is listed in Table 1. A prototype spiral UTE VIBE sequence was used for data acquisition. Parameters, settings, reconstruction methods, and number of coils are listed in Table 3. Lung CT was performed with a 128-slice CT scanner (Brilliance iCT, Philips Healthcare, Cleveland, OH, USA) with 120 kVp 119-235 mA (modulated) and reconstructed coronally in 3 mm slices. One interpreting radiologist was blinded to the exact location of the lung nodules. CT was used as the reference standard to determine nodule size and location, and to differentiate solid, part-solid, and non-solid nodules. The sizes of the nodules were compared on MRI-PET and CT. The detection rate and SNR were calculated for the MRI scanners.Results
Image quality was initially compared between spiral iPAT factors of 1 and 2 in the 3T MR-PET scanner. A spiral iPAT factor of 2 showed stripe artifacts in some of the slices, which was solved when switching off the spiral iPAT factor to 1 (Figure 1). Therefore, subsequent scans had the spiral iPAT factor set to 1 (Table 3). Figures 2 and 3 show the representative images of solid and non-solid nodules in both 3T MR-PET and low-dose CT. Second, nodule detection rates from both scanners were analyzed (Table 2). In the 3T MR-PET scanner, the free-breathing spiral UTE VIBE sequence showed a detection rate of 67% for both solid and non-solid nodules, whereas the breath-hold sequence showed a detection rate of 89%. One non-solid nodule could not be detected in the 3T MR-PET scanner, either in the free-breathing or breath-hold spiral UTE VIBE sequences. The 1.5T scanner showed a higher nodule detection rate in solid, non-solid, and part-solid nodules compared with the 3T MR-PET. Third, the size of the solid nodules between 3T MR-PET and CT was compared using a Bland-Altman plot. The bias was -2.12 ± 4.51 [mm] compared with free-breathing spiral UTE VIBE and CT, and it was -1.25 ± 2.92 [mm] compared with breath-holding spiral UTE VIBE and CT (Figure 4). Furthermore, the SNR in the 3T MR-PET for free-breathing and breath-hold spiral UTE VIBE were 15 and 16, respectively, which were smaller compared with those obtained with the 1.5T scanner.Discussion
Pulmonary nodule detection with spiral UTE VIBE sequence was first used with the 3T MR-PET scanner. A stripe artifact appeared but was suppressed when switching off spiral iPAT and changing to Non-Uniform Fourier Transform (NUFT) reconstruction. The artifacts may have resulted from fewer coil elements of the body and spine matrix coil. In the MR-PET scanner, the RF coil degraded PET image quality through attenuation and scatter. Development of coils with a higher channel count for the MR-PET scanner is challenging and requires a different approach compared to conventional MR coils. Therefore, we used MR- and PET-compatible coils which have fewer coil elements compared with the coils in MR-only scanners. Our results indicated that the spiral UTE VIBE sequence acquired good image quality even with fewer coil elements when suppressing the acceleration factor. The SNR tended to be higher in the 1.5T scanner, which is reasonable when considering that the 3T MR-PET scanner has fewer coil elements. Despite decreased SNR, the detection rate of the solid lung nodules remained high for the breath-holding UTE sequence. The breath-holding spiral UTE sequence may be beneficial for use in the lung health-check MRI examination for nodule detection to manage the total scan time, solving one of the problems of the whole-body health-check examination.Conclusion
Our study results suggest that the use of spiral UTE VIBE enables the detection of solid lung nodules in the 3T MR-PET system. Although previous research has been performed using spiral UTE VIBE with higher coil elements, our study suggests that spiral UTE VIBE can work even with fewer coil elements.Acknowledgements
No acknowledgement found.References
1. Huang YS, Niisato E, Su MYM, Stemmer A, Chen JS, Chang YC. Pulmonary nodule detection using ultra-short TE (UTE) with a 3D variable-TE stack-of-spirals sequence. Joint Annual Meeting ISMRM – ESMRMB, Paris, France; 2018. #4364.
2. Sałyga A, Guzikowska-Ruszkowska I, Czepczyński R1, Ruchała M. PET/MR-a rapidly growing technique of imaging in oncology and neurology. Nucl Med Rev Cent East Eur. 2016;19(1):37-41
3. Fraioli F, Screaton NJ, Janes SM, Win T, Menezes L, Kayani I, Syed R, Zaccagna F, O'Meara C, Barnes A, Bomanji JB, Punwani S, Groves AM. Non-small-cell lung cancer resectability: diagnostic value of PET/MR. Eur J Nucl Med Mol Imaging. 2015 Jan;42(1):49-55
4. Ohno Y, Koyama H, Matsumoto Y, et al. Lung MR imaging with ultra-short TE at 3.0T system: capability for pulmonary functional loss due to COPD. Proc. Intl. Soc. Mag. Reson. Med. 2010;18:203.
5. Fielden S, Mugler J, Miller W, Stemmer A, Pfeuffer J, Kiefer B, Meyer C. A variable-TE stack-of-spiral sequence for 3D UTE imaging. Proc. Intl. Soc. Mag. Reson. Med. 2016;24:1062
6. Lustig M, Pauly JM. SPIRiT: Iterative self-consistent parallel imaging reconstruction from arbitrary k-space. Magn Reson Med. 2010;64(2):457-471.
7. Mugler JP, Meyer CH, Pfeuffer J, Stemmer A, Kiefer B. Accelerated Stack-of-Spirals Breath-hold UTE Lung Imaging; In: Proceedings of the 25th Annual Meeting of ISMRM, Honolulu, Hawaii; 2017. p. 4904
Figures
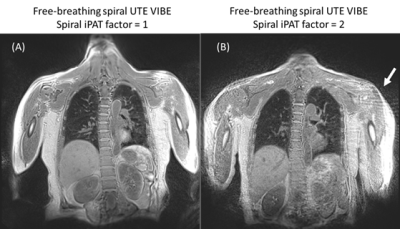
Figure 1. Free-breathing spiral UTE VIBE images without the use of spiral iPAT factor of 1 (A) or spiral iPAT factor of 2 (B), from the same patient. Stripe artifact is observed (white arrow) and is suppressed when switching off iPAT.
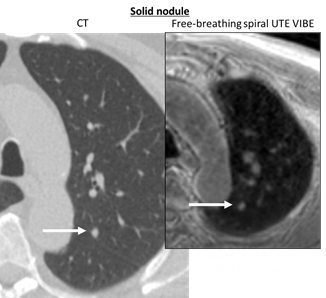
Figure 2. Solid nodules detected by free-breathing spiral UTE VIBE and CT. The arrow shows the solid nodule.
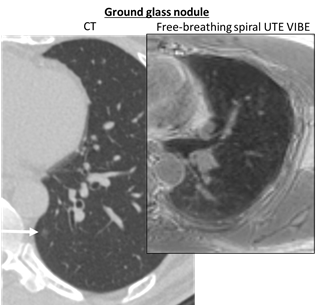
Figure 3. Non-solid nodule detected by CT that was unable to be detected with free-breathing spiral UTE VIBE. The arrow shows the non-solid nodule.
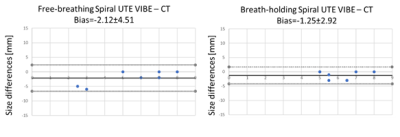
Figure 4. Bland-Altman plot depicts the differences in the solid nodule size between 3T MR-PET and reference CT images. Smaller bias was seen for breath-holding spiral UTE VIBE.
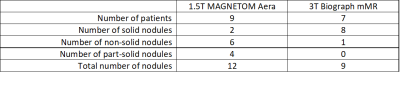
Table 1. Patient demographics (number of each nodule is confirmed by CT)
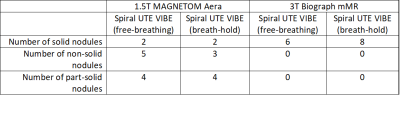
Table 2. Number of nodules in Table 1 detected by MR scanners
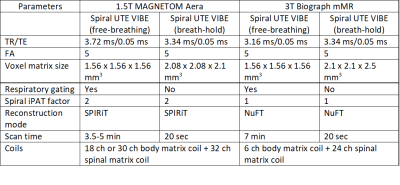
Table 3. Comparison of parameters for spiral ultrashort-TE sequence acquired using the 1.5T MR and 3T MR-PET scanners.