2343
Quantify the Influence of Smoking on Pulmonary Structure and Function in Lung Cancer Patients using Hyperpolarized 129Xe MR
Qian Zhou1, Haidong Li1, Qiuchen Rao1, Junshuai Xie1, Xiuchao Zhao1, He Deng1, Lei Shi1, Xianping Sun1, Yeqing Han1, Dongshan Han2, Xin Lou2, Chaohui Ye1, and Xin Zhou1
1National Center for Magnetic Resonance in Wuhan, Wuhan Institute of Physics and Mathematics, Innovation Academy of Precision Measurement Science and Technology, Chinese Academy of Sciences-Wuhan National Laboratory for Optoelectronics, Wuhan, China, 2Department of Radiology, Chinese PLA General Hospital, Beijing, P. R. China, Beijing, China
1National Center for Magnetic Resonance in Wuhan, Wuhan Institute of Physics and Mathematics, Innovation Academy of Precision Measurement Science and Technology, Chinese Academy of Sciences-Wuhan National Laboratory for Optoelectronics, Wuhan, China, 2Department of Radiology, Chinese PLA General Hospital, Beijing, P. R. China, Beijing, China
Synopsis
Pulmonary diseases, such as lung cancer, usually result in changes of pulmonary structure and function. To assess these changes, gas exchange across the respiratory membrane and gas diffusion in the alveoli can be quantified using hyperpolarized 129Xe MR via CSSR and DWI in lung cancer patients, The significant differences were found in mean exchange time constant(T) and septal wall thickness(d) between smoking and non-smoking lung cancer patients, indicating the impact of smoking. The results manifested that the hyperpolarized 129Xe MR is a promising method for optimizing radiation therapy in the future.
INTRODUCTION:
Lung cancer is the chief death cause in malignancy tumors worldwide and smoking is considered as one of the main reasons for lung cancer. The general clinical imaging techniques, including chest X-ray, CT and ECT could measure the changes of lung parenchyma caused by cancers. However, these imaging techniques are unable to measure pulmonary function changes without ionizing radiation, which have a potential effect on human health. Hyperpolarized noble gas lung MRI is a noninvasive, radiation-free technique that permits the acquisition of high-resolution lung images1. This technique is able to provide the information about pulmonary morphology and gas exchange properties, which is sensitive to pulmonary structure and functional changes associated with a number of pulmonary diseases2. In this work, we assessed the influence of smoking on pulmonary structure and gas exchange function among lung cancer patients.METHODS:
Eight patients (aged 55-79) with histologically confirmed lung cancer were scanned at 1.5T human MRI scanner using a homebuilt transmit‐receive vest RF coil (17.61 MHz for 129Xe), and five of them had a history of smoking. All the patients underwent HP 129Xe multi-b diffusion-weighted imaging (DWI) (b = 0, 10, 20, 30, and 40 s/cm2) and chemical shift saturation recovery (CSSR) spectroscopy scanning. All subjects inhaled 1 L of gas mixture (45% xenon +55% N2) from functional residual capacity (FRC) for the CSSR and DWI experiments separately. DWI data employed a gradient echo diffusion sequence with following acquisition parameters: slice thickness = 30 mm, TR/TE = 13.9/10.9 ms, flip angle = 9°, in-plane resolution = 4*4 mm2. The pulmonary microstructural parameters, such as external radius (R), internal radius (r), extracted using HP 129Xe DWI data3. For the acquisition of CSSR data, the exchange time (τ) ranged from 4 ~ 700 ms with a total scan time of 5.2s. Physiological parameters, including exchange time constant (T) and pulmonary septal wall thickness (d), were extracted by fitting CSSR data to the model of xenon exchange (MOXE)4.RESULTS:
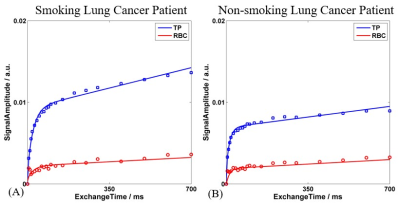
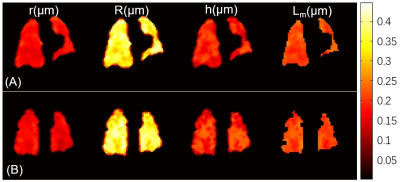
Figure 1 showed the measured and fitted TP and RBC signal as a function of exchange time (τ) for the lung cancer patients with history of smoking (A) and without history of smoking (B). Significant differences were found in exchange time and septal wall thickness between the smoking and non-smoking lung cancer patients (p < 0.01), and the mean exchange time was 31.86 ± 5.88 ms and 16.83 ± 3.33 ms in both groups. 129Xe-DWI results showed no significant differences between groups. The maps of lung microstructural parameters are similar and homogeneous in both groups, as shown in figure 2.DISCUSSION and CONCLUSION:
The results of HP 129Xe CSSR indicate that the mean exchange time constant (T) and septal wall thickness (d) could be used to assess the influence of smoking on the physiological changes among the lung cancer patients. The significant increase of the mean exchange time constant (T) and septal wall thickness (d) in smoking groups were most possibly due to the smoking-induced lung injury, which means smoking may has prominent influence on lung physiological changes. Our study indicates HP 129Xe is sensitive to smoking-induced degradation of lung function and provides insights into quantifying of disease severity and monitoring treatment response.Acknowledgements
This work was supported by National Key R&D Program of China (2018YFA0704000), National Natural Science Foundation of China (81625011, 91859206, 21921004, 81601491), Key Research Program of Frontier Sciences, CAS (QYZDY-SSW-SLH018) and Hubei Provincial Natural Science Foundation of China (2017CFA013, 2018ACA143).References
- Qing K, Mugler JP, III, Altes TA, et al. Assessment of lung function in asthma and COPD using hyperpolarized Xe-129 chemical shift saturation recovery spectroscopy and dissolved-phase MRI. NMR Biomed 2014; 27: 1490-1501.
- Li H, Zhang Z, Zhao X, et al. Quantitative evaluation of radiation-induced lung injury with hyperpolarized xenon magnetic resonance. Magn Reson Med 2016; 76: 408-416.
- Sukstanskii AL, Yablonskiy DA. Lung morphometry with hyperpolarized Xe-129: theoretical background. Magn Reson Med 2012; 67: 856-866.
- Chang YV. MOXE: a model of gas exchange for hyperpolarized Xe-129 magnetic resonance of the lung. Magn Reson Med 2013; 69: 884-890.