2336
Diffusion-Weighted Breast MRI in the Supine Position1Radiology, Stanford University, Stanford, CA, United States, 2Veterans Administration Health Care System, Palo Alto, CA, United States
Synopsis
Diffusion-Weighted Imaging has shown strong potential to be the centerpiece of a breast MRI screening protocol that does not require a contrast injection. Breast MRI is conventionally performed in the prone position but supine positioning could increase patient comfort and alignment of MRI findings with other interventional procedures. Here we investigate six multi-shot DWI breast protocols with supine positioning in assymptomatic volunteers. Over all images quality and trade-offs between motion artifacts, distortion and images sharpness are characterized.
Introduction
Conventional breast MRI in performed in the prone position. Supine breast MRI has been investigated for alignment of imaging findings with breast anatomy during interventional procedures and could greatly increase patient comfort for screening MRI [1-4]. Diffusion-weighted MRI (DWI) achieves high sensitivity for the detection of breast cancer without the need for an intravenous contrast agent but has not been investigated extensively in the supine position. Motion and B0 inhomogeneity, both of which can greatly affect DWI image quality will vary between the prone and supine position. In this work we investigate supine DWI in the breast with multi-shot DWI methods. As supine DWI in the breast has not been extensively investigated, we focus on characterizing over all image quality and trade-offs between motion compensation strategies, distortion and signal level.Materials and Methods
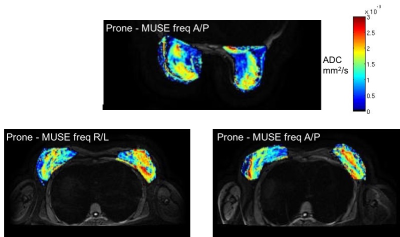
Multiplexed Sensitivity Encoding (MUSE)5 is a multi-shot acquisition strategy which offers reduced image distortions and makes use of parallel imaging to estimate motion-induced phase. Convex Optimized Diffusion-Encoding (CODE)6 makes use of convex optimization to generate minimum time duration diffusion encoding gradients with flexibility to add higher order gradient moment nulling. Three different supine DWI protocols were investigated 1) MUSE; 2) MUSE with respiratory-gating; 3) Multi-shot DWI with Convex Optimized Diffusion-Encoding (CODE). To investigate trade-offs between distortion and propagation of motion artifacts, each acquisition was acquired with the frequency encoding direction in the right/left (R/L) and anterior/posterior (A/P) directions for a total of 6 supine DWI protocols.Three asymptomatic breast volunteers were scanned in the supine position with the six multi-shot DWI strategies described above. Scans were performed on a 3T scanner (GE Healthcare SIGNA® Premier, Waukesha, WI) using a 32-channel torso coil A plastic support was placed under the coil to keep the coil from compressing the breast tissue. The imaging parameters used for all acquisitions are detailed in Figure 1. After supine scanning each volunteer was then scanned in the prone position with a 16-channel breast coil (Sentinelle by In Vivo) using the MUSE 4-shot acquisition with A/P frequency encoding and no parallel imaging as the protocol most representative of current clinical multi-shot prone DWI protocols. A single shim volume extending across both breasts was used in the supine position while a dual volume shim with a separate volume centered on each breast was utilized in the prone acquisition. An GRE acquisition was also performed in the supine position to provide a reference for degree of distortion in the DWI images. ADC maps were calculated for the prone acquisition and the two non-gated MUSE acquisitions. Signal in fibroglandular tissue was measured. Overall image quality including sharpness, presence of motion artifact, and inhomogeneity were assessed qualitatively between protocols.
Results
All supine breast MRI protocols achieved over all good image quality without severe motion artifacts or distortion. Images sharpness was improved with frequency encode R/L versus A/P (Figure 2) possibly due to the lower number of phase-encodes required with the smaller FOV A/P. Resolution was also improved by incorporating respiratory gating into the MUSE protocol. The CODE images demonstrated sharp depiction of lesion morphology but also some loss of contrast. Some areas of small inhomogeneity may be present in the breast tissue but the supine DWI images generally compared will the reference GRE images (Figure 3). While strict signal measurements are not a basis to establish conclusions about the comparison of these methods they serve as a starting point for continued characterization of the methods, in particular the consistent signal difference between the A/P and R/L protocols (Figure 4). Finally, ADCs reflective of those expected for normal fibroglandular tissue were calculated with the supine protocols (Figure 5).Discussion and Conclusions
In this work we investigated the feasibility of performing DWI in the breast with supine positioning of the patient. Development of a breast MRI protocol which does not require a contrast injection is imperative for increasing accessibility and compliance of screening for breast cancer and DWI has shown strong potential to be the centerpiece of such a protocol. Screening in the supine position could greatly increase comfort but the challenges of DWI, most notably the balance of motion susceptibility and image distortion will vary between prone and supine positions. The 6 supine DWI protocols investigated in this work all demonstrated good over all image quality and analysis of more specific image characteristics provide a starting point for the further refinement of the protocols. While more work remains these results encourage continued investigation of supine DWI in the breast.Acknowledgements
We acknowledge NIH R01 EB009055, NIH K24-AR062068-07, and research support from GE Healthcare.References
1. Siegler et al, Eur J Rad 2012 81S1 S153-S155.
2. Janssen et al, Acad Radiol 2017 24(7) 818-825.
3. Gombos et al, Radiology 2016 281(3) 720-729.
4. Batumalai et al, Radio and Onc 2016 119 57-60.
5. Chen et al, Neuroimage 2013 72:41-47.
6. Aliotta et al, MRM 2017 77:717-729.
Figures
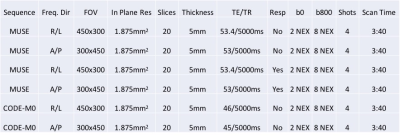
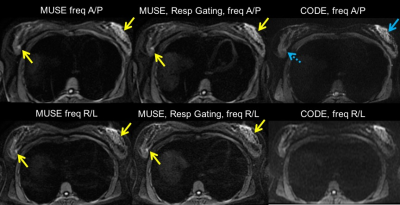
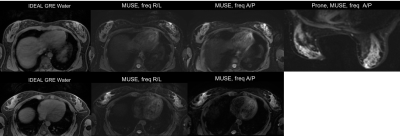
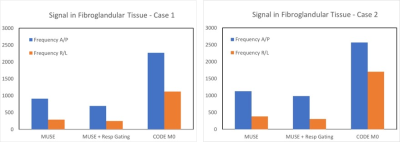
Figure 4. Measurement of fibroglandular tissue signal from 2 cases. MUSE and CODE use different reconstruction techniques so this measure should not be used to draw conclusions between the two. However,it can be informative within each method. Signal in fibroglandular tissue is lower with frequency R/L versus A/P. Some of the signal loss may be due to the propagation of cardiac motion artifact across the breast tissue when frequency encode L/R. The much higher signal in the CODE images highlights the advantage of a shorter echo time that is achieved with the optimized gradient wavefoms.