2335
Approach for building a DWI dedicated lexicon for breast cancer1Radiology, Kitano Hospital, The Tazuke Kofukai Medical Research Institute, Osaka, Japan, 2Diagnostic Imaging and Nuclear Medicine, Kyoto University Graduate School of Medicine, Kyoto, Japan, 3Breast Surgery, Kitano Hospital, The Tazuke Kofukai Medical Research Institute, Osaka, Japan
Synopsis
Our proposed DWI reading method based on the BI-RADS lexicons from multiple b-value images had comparable diagnostic performance to the standard BI-RADS. DWI reading method tended to show with higher specificity, and might increase diagnostic confidence in differentiating malignant and benign breast tumors. Excellent to substantial agreement was observed for DWI reading, and substantial agreement was found for mass type classifications between DWI and BI-RADS. Significant difference found in lesion conspicuity between malignant and benign tumors and ADC values assessmet may also provide confidence in tumor characterization.
Introduction
DWI has been widely used for the diagnosis and monitoring of breast lesions. Although DWI for clinical breast MRI, it is not included in the BI-RADS-MRI assessment 1-3. However, integration of DWI and DCE has been shown to improve specificity 2, 4. ADC calculation, which allows differentiation of malignant and benign breast lesions, is also often not fully considered in routine clinical reading. Evaluation of breast tumor morphology by DWI has been attempted 5, 6, with slight to fair agreement between DWI-reading and BI-RADS. Here, we propose a DWI-reading method based on the BI-RADS lexicons from multiple b-value images. Diagnostic performance was evaluated in comparison with standard BI-RADS and ADC values.Material and Methods
-Study population and acquisition-This prospective study was approved by our institutional review board and included 46 women suspected with breast cancer. Eighty-six breasts (15 malignant, 14 benign, 57 no findings) were further analyzed. Breast MRI was performed using a 3-T system (Achieve 3T; Philips) equipped with a dedicated 7-channel breast array coil. DWI was acquired using five b-values of 0, 200, 800, 1000, and 1500 s/mm2; repetition time/echo time, 12500/79 ms; flip angle, 90°; field of view, 350 × 350 mm; matrix, 112×145; slice thickness, 4.0 mm; and acquisition time, 5 min 25 s.
-DWI-based reading-
Two independent radiologists, blinded to all other information, assessed lesion characteristics and normal breast tissue solely on the DW images according to an adjusted BI-RADS lexicon for lesion classification. This was followed by a standard DCE (example shown in Figure 1).
-ADC and measurement-
ADC and shifted ADC (sADC) values were measured by two independent radiologists, calculated as: = [SnLb/SnHb/(Hb-Lb) [1], where is the low key b-value and Hb is the high key b-value 7. Different [Hb, Lb] pairs were evaluated.
Results
The diagnostic performance of radiologists A and B is summarized in Table 1. Overall, tended to be inferior in DWI than with BI-RADS, while superior specificity and comparable sensitivity, PPV, and NPV were achieved on DWI-reading. Excellent interobserver agreement was obtained in assessment of BI-RADS categories, lesion type, and FGT DWI (k=0.87, 0.86, 0.80, Table 2). Substantial interobserver agreement was obtained for mass margin, and internal pattern (k=0.78, 0.66, 0.68). Agreement between DWI and DCE-MRI was fair to moderate for FGT and (k=0.29–0.47), and fair for mass margin and internal pattern (k=0.29–0.38). Interobserver agreement was excellent for lesion score (ICC>0.90) and ADC or values (ICC: 0.90–0.97); therefore, each value was averaged for further analysis. Lesion scores in benign tumors were significantly lower at b=1500 s/mm2Discussion
Our proposed DWI reading methods achieved diagnostic performance comparable to the standard BI-RADS. With higher specificity, DWI reading with multiple b-values has the potential to increase diagnostic confidence in differentiating malignant and benign breast tumors. Interobserver agreement for DWI reading between two independent radiologists was excellent to substantial, and mass type classifications showed substantial agreement between DWI and BI-RADS. These results suggest that DWI reading methods might beConclusion
DWI reading methods showed comparable diagnostic performance to standard BI-RADS, and they might increase diagnostic confidence in differentiating malignant and benign breast tumors.Acknowledgements
This research was supported by AMED under Grant Number JP18ck0106454.References
1. Shi RY, Yao QY, Wu LM, Xu JR. Breast Lesions: Diagnosis Using Diffusion Weighted Imaging at 1.5T and 3.0T-Systematic Review and Meta-analysis. Clin Breast Cancer. 2018; 18e305-e320.
2. Zhang L, Tang M, Min Z, Lu J, Lei X, Zhang X. Accuracy of combined dynamic contrast-enhanced magnetic resonance imaging and diffusion-weighted imaging for breast cancer detection: a meta-analysis. Acta Radiologica. 2016; 57:651-660.
3. Iima M, Honda M, Sigmund EE, Ohno Kishimoto A, Kataoka M, Togashi K. Diffusion MRI of the breast: Current status and future directions. Journal of Magnetic Resonance Imaging. 2019.
4. Goto M, Le Bihan D, Yoshida M, Sakai K, Yamada K. Adding a Model-free Diffusion MRI Marker to BI-RADS Assessment Improves Specificity for Diagnosing Breast Lesions. Radiology. 2019; 292:84-93.
5. Radovic N, Ivanac G, Divjak E, Biondic I, Bulum A, Brkljacic B. Evaluation of Breast Cancer Morphology Using Diffusion-Weighted and Dynamic Contrast-Enhanced MRI: Intermethod and Interobserver Agreement. J Magn Reson Imaging. 2018.
6. Kul S, Metin Y, Kul M, Metin N, Eyuboglu I, Ozdemir O. Assessment of breast mass morphology with diffusion-weighted MRI: Beyond apparent diffusion coefficient. J Magn Reson Imaging. 2018; 48:1668-1677.
7. Iima M, Le Bihan D. Clinical Intravoxel Incoherent Motion and Diffusion MR Imaging: Past, Present, and Future. Radiology. 2016; 278:13-32.
Figures
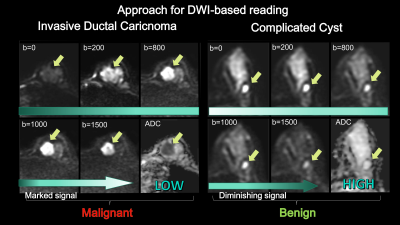
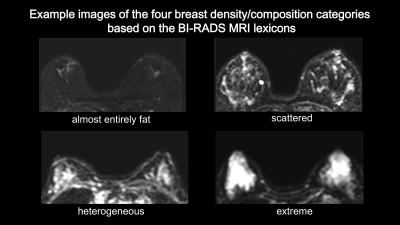
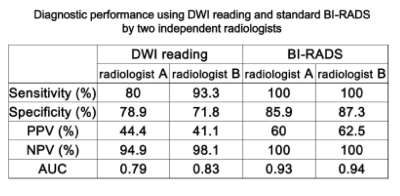
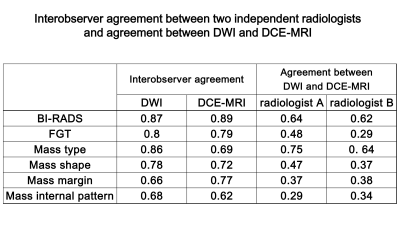
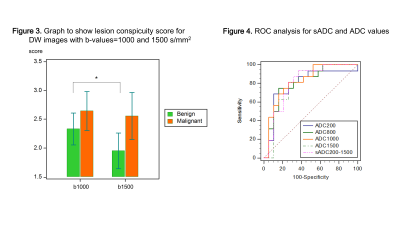
Figure 3. Graph to show for DW images with b-values=1000 and 1500 s/mm2. Lesion score was significantly lower in benign lesions at b=1500 s/mm2, while no significant difference was observed in malignant breast lesions.
Figure
4. ROC analysis for