2303
Assessment of the Ventilation Rate allows for Interindividual Comparability of Ventilation Inhomogeneity in Functional 3D-UTE Lung MRI1Department of Diagnostic and Interventional Radiology, University Hospital Wurzburg, Wurzburg, Germany, 2Application Development, Siemens Healthcare GmbH, Würzburg, Germany, 3Department of Pediatrics, University Hospital Wurzburg, Wurzburg, Germany
Synopsis
Lung imaging with single-breath-hold 3D-UTE MRI allows for lung function analyses such as fractional ventilation (FV). Despite being a promising technique for unenhanced functional imaging, its limited interindividual comparability due to variable breathing depths has been a major drawback. Referencing the voxelwise FV to the mean FV (entire lung) provides the ventilation rate, which can be used for inter-/intraindividual comparison. We demonstrate that the distribution width of the ventilation rate strongly correlates to the ventilation inhomogeneity in patients with cystic fibrosis as measured by the lung clearance index, which makes it a promising parameter for analysis of lung ventilation.
Introduction
Proton-based non-contrast-enhanced lung MRI allows for analysis of functional imaging parameters such as fractional ventilation (1). By using MRI sequences with ultrashort echo-times (UTE), a high signal-to-noise ratio can be achieved in spite of low proton density and fast signal decay in the lungs. In addition, highly effective stack-of-spiral trajectories enable significantly accelerated image acquisition within single breath-holds (2,3). By analyses of the signal change between inspiration and expiration, the fractional ventilation (FV) can be calculated, which, however, is highly dependent on the individual breathing depth and therefore lacks comparability. Rather than evaluating the mean values of the whole lung, it is promising to quantify regional ventilation defects (4,5). In cystic fibrosis (CF), mucus accumulation in the airways leads to progressive decline of lung function. For disease management, conventional pulmonary function tests (PFT) are used for monitoring lung function in CF patients. Additionally, the multiple breath washout (MBW) test is used to determine the ventilation inhomogeneity, which has been shown to be a more sensitive marker for early disease progression in CF when compared to parameters of PFT. The purpose of this study was to determine the ventilation inhomogeneity from 3D-UTE functional lung MRI in patients with cystic fibrosis.Methods
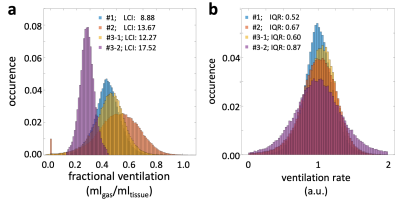
3D-UTE MR imaging of the lungs was performed on a 3T MR scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) using a prototypical 3D-UTE stack-of-spirals sequence (2) with a dual-density trajectory (3), iPAT factor 2 and SPIRiT reconstruction (6) using the following parameters: TE = 0.05 ms; TR = 2.35 ms; flip angle = 5°; nonselective-hard-pulse duration = 60 µs; FOV = 600 mm x 600 mm; spiral interleaves = 264; readouts per spiral = 265; resolution = 2.3 x 2.3 x 2.3 mm3; number of partitions = 102 ± 14. Twenty patients with cystic fibrosis underwent MR imaging in inspiration and expiration within a single breath-hold per measurement and a pause in between, leading to a total acquisition time of 40 s. Two patients underwent an additional follow-up examination one month later. Images were co-registered (7) and segmented fully automatically (8) to obtain voxelwise fractional ventilation (FV) as proposed earlier (1). The ventilation rate was obtained by normalization of the FV (referenced to the whole-lung mean FV), where values < 1 indicate a ventilation lower and values > 1 a ventilation higher compared to the entire lung. The distribution width of the ventilation rate was evaluated by the interquartile range (IQR) and compared between groups. Pulmonary function tests (PFT) and nitrogen multiple-breath-washout test (MBW) was performed the same day. IQR of the ventilation rate was correlated with results of PFT and the lung clearance index (LCI) from MBW tests.Results
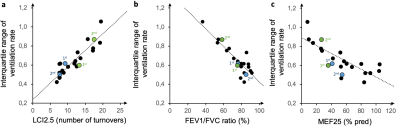
Figure 1 exemplarily provides the distribution of FV before normalization and the ventilation rate (after normalization) for 4 study participants, illustrating the interindividual comparability of the ventilation rate. IQR of the ventilation rate correlated positively with the markers for airway obstruction MEF25 and FEV1/FVC ratio (Tiffeneau index) with Spearman’s r = 0.7/0.8, respectively, and strongly with the LCI2.5% (r = 0.9) (Figure 2). The results of two patients who underwent an additional follow-up examination indicate good intraindividual comparison of the ventilation rate, demonstrated by good correlation with PFT and MBW. Likewise, the respective changes in lung function could be monitored by UTE-MRI (Figure 2, green and blue marks, initial and follow-up is indicated as 1st and 2nd). Figure 3 provides exemplary ventilation rate maps of the initial and follow-up examination of one patient.Discussion
In breath-hold 3D-UTE lung MRI, the inter- and intraindividual comparability of the fractional ventilation is hindered by the variability of individual breathing depths. Normalization of the voxelwise FV to the mean FV of the entire lung yields the ventilation rate, which is independent from the breathing depth and enables an inter- and intraindividual comparison. The distribution width of the ventilation rate can be evaluated by the interquartile range (IQR), which correlated positively to obstruction markers from PFT and strongly with the LCI, a marker for ventilation inhomogeneity. The follow-up examinations of two patients indicate a good repeatability for assessment of the distribution width of the ventilation rate.Conclusion
Single-breath-hold 3D-UTE MRI is a promising tool for non-contrast-enhanced functional lung imaging. To overcome the variability of breathing, the ventilation rate can be determined, which allows inter- and intraindividual comparability and enables monitoring of the ventilation inhomogeneity.Acknowledgements
No acknowledgement found.References
1. Zapke M, Topf H-G, Zenker M, Kuth R, Deimling M, Kreisler P, Rauh M, Chefd’hotel C, Geiger B, Rupprecht T. Magnetic resonance lung function – a breakthrough for lung imaging and functional assessment? A phantom study and clinical trial. Respir. Res. 2006;7:106.
2. Mugler JP, Meyer CH, Pfeuffer J, Stemmer A, Kiefer B. Accelerated Stack-of-Spirals Breath-hold UTE Lung Imaging. Proc. Intl. Soc. Mag. Reson. Med. 2017;p. 4904.
3. Meyer CH, Zhao L, Lustig M, Jilwan-Nicolas M, Wintermark M, Mugler JP, Epstein FH. Dual-Density and Parallel Spiral ASL for Motion Artifact Reduction. Proc. Intl. Soc. Mag. Reson. Med 2011;64:3986.
4. Kaireit TF, Sorrentino SA, Renne J, et al. Functional lung MRI for regional monitoring of patients with cystic fibrosis. PLoS One 2017.
5. Veldhoen S, Weng AM, Knapp J, et al. Self-gated Non–Contrast-enhanced Functional Lung MR Imaging for Quantitative Ventilation Assessment in Patients with Cystic Fibrosis. Radiology 2017;283:242–251.
6. Lustig M, Pauly JM. SPIRiT: Iterative self-consistent parallel imaging reconstruction from arbitrary k-space. Magn. Reson. Med. [Internet] 2010;64.
7. Klein S, Staring M, Murphy K, Viergever MA, Pluim JPW. Elastix: A toolbox for intensity-based medical image registration. IEEE Trans. Med. Imaging 2010.
8. Weng AM, Kestler C, Kunz AS, Veldhoen S, Bley TA, Köstler H, Wech T. Deep Learning Assisted Fully Automatic Post-Processing for Quantitative Lung MRI. In: Proc. Intl. Soc. Mag. Reson. Med. 27. ; 2019. p. 1720.
Figures
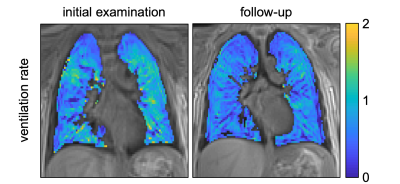
Representative slices of ventilation rate maps from patient #2 (same as Figure 2). The initial MRI was acquired during acute exacerbation and decreased lung function. After antibiotic and steroid therapy, the patient recovered (lung function was restitutio ad integrum), and a decreased ventilation inhomogeneity and IQR was observed in follow-up examination (initial IQR: 0.61; follow-up IQR: 0.50).