2299
Feasibility study of nodule conspicuity for lung screening using ultrashort echo time MRI1Department of Radiology, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan, 2Department of Radiology, The University of Tokyo Hospital, Tokyo, Japan, 3Department of Computational Diagnostic Radiology and Preventive Medicine, The University of Tokyo Hospital, Tokyo, Japan
Synopsis
Pulmonary MRI with ultrashort echo time (UTE) is expected to be an alternative to low-dose CT for lung screening. In this study, the feasibility of breath-hold (BH) and respiratory triggered (RT) scans with UTE was investigated. In total, 229 lung MRI examinations that were composed of 136 examinations with a solid nodule (SN) and 93 examinations with a ground-glass nodule (GGN) were evaluated. Both results of qualitative and quantitative assessment suggested that SN was more clearly depicted than GGN. BH scan in pulmonary MRI should be more suitable for lung screening than RT scan.
INTRODUCTION
The National Lung Screening Trial Research Team revealed that low-dose CT was useful to reduce mortality from lung cancer.1-3 Recently, it has been suggested that pulmonary MRI with ultrashort echo time (UTE) may be effective in lung screening without radiation exposure instead of low-dose CT.4-7 So far, however, no study has compared the effect of breath-hold (BH) with that of respiratory triggered (RT) sequence in pulmonary MRI. The purpose of this study was to evaluate the usefulness of BH sequence in light of visualization and nodule conspicuity and to investigate the feasibility of BH and RT sequences for lung screening.METHODS
Out of 2,281 lung MRI examinations performed in a comprehensive health screening program, 229 examinations (159 men and 70 women; mean age, 65.3 years; age range, 41–88 years) with one or more pulmonary nodules on low-dose CT were retrospectively evaluated. Data were obtained at a medical checkup institution from March 2018 to November 2018. The UTE images were acquired on a 3 T MR scanner (MAGNETOM Skyra, Siemens Healthineers, Erlangen, Germany) in two ways including BH and RT. Parameters for BH were as follows: TE, 0.05 ms; repetition time (TR), 2.66 ms; field-of-view, 600 x 600 mm2; flip angle, 2.5°; matrix size, 352 x 352; slice thickness and interval, 1.7 mm and 1.7 mm; and scan time, 22 seconds. Parameters for RT were as below: TE, 0.05 ms; TR, 3.27 ms; field-of-view, 600 x 600 mm2; matrix size, 384 x 384; slice thickness and interval, 1.56 mm and 1.56 mm; and scan time, 300 seconds. The size of nodules was more than 5 mm, and the largest nodule per participant was a candidate for the following assessment.Qualitative assessment of normal structures and nodules
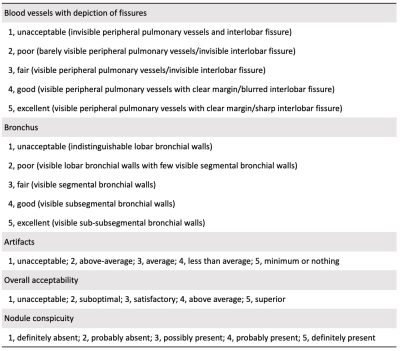
Two radiologists (with 25 and 5 years of experience in chest imaging, respectively) independently evaluated UTE images in terms of visualization of blood vessels and bronchus, degree of artifacts, overall acceptability, and nodule conspicuity including the judgment of either a solid nodule (SN) or a ground-glass nodule (GGN). A five-point scale was used to rate the score of each category (Table 1).6
Quantitative assessment of nodules
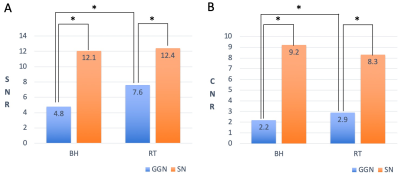
The latter radiologist measured the signal intensity (SI) of nodule, tracheal lumen, and lung parenchyma using a circular region of interest, and investigated a signal-to-noise ratio (SNR) and a contrast-to-noise ratio (CNR) of nodules. The SNR was calculated as mean SI (nodule)/standard deviation of the SI (tracheal lumen), and the CNR as mean SI (nodule) – mean SI (lung)/standard deviation of the SI (tracheal lumen).
Statistical analysis
Statistical analyses were performed using SPSS package version 26.0 (SPSS Inc.). Wilcoxon signed rank test was used to compare qualitative scores of each normal structure and nodule type between BH and RT as well as SI differences of the SNR and CNR between these two sequences. Mann-Whitney U test was used to compare SI differences of the SNR and CNR between SN and GGN. Interobserver performance for qualitative scores in each category was assessed by the kappa coefficient, which was interpreted as follows: 0–0.20, poor; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, good; and 0.81–1.00, almost perfect. P values of less than 0.05 were considered as statistical significance.
RESULTS
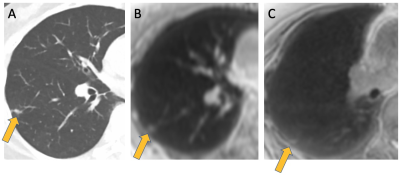
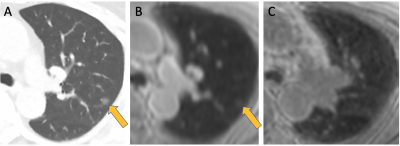
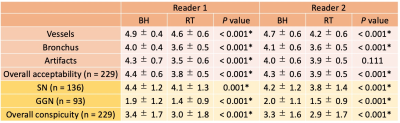
As a result, 229 examinations were split into 136 examinations for SN (Figure 1) and 93 examinations for GGN (Figure 2). Table 2 shows the result of the qualitative assessment of normal structures, artifacts, and nodule conspicuity by two independent readers. The five-point scale in each category between BH and RT was statistically significant except for the degree of artifacts by the reader 2. Overall, the grade of BH was higher than that of RT. The interobserver performance was almost perfect. The quantitative assessment of nodules is illustrated in Figure 3. The SNR and CNR of SN were significantly higher than those of GGN, which corresponded to the result of qualitative grading shown in Table 2.DISCUSSION
The feasibility of BH sequence in pulmonary MRI for lung screening was revealed. It is true that RT scan takes more time and is troublesome especially for the people with great respiratory fluctuation. However, several nodules were more clearly depicted in RT than BH. Thus, the additional scan of RT may be required in the time-rich case, although BH scan should be the first choice for lung screening.The above result suggests that pulmonary MRI may have possibilities for lung disease screening. At present, however, GGN was more difficult to be detected than SN. Advanced sequences are desirable to detect GGN.
CONCLUSION
Both results of qualitative and quantitative assessment indicated that SN was more clearly depicted than GGN. BH scan in pulmonary MRI should be more suitable for lung screening than RT scan.Acknowledgements
We gratefully acknowledge thoughtful comments of Dr. Katsutoshi Murata and Dr. Alto Stemmer from Siemens Healthineers. There are no conflicts of interest with any authors.References
1. The National Lung Screening Trial Research Team. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. The New England Journal of Medicine 2011;365(5):395-409.
2. Yanagawa M, et al. Pulmonary nodules: Effect of adaptive statistical iterative reconstruction (ASIR) technique on performance of a computer-aided detection (CAD) system—Comparison of performance between different-dose CT scans. European Journal of Radiology 2012;81:2877-86.
3. Nomura Y, et al. Effects of Iterative Reconstruction Algorithms on Computer-assisted Detection (CAD) Software for Lung Nodules in Ultra-low-dose CT for Lung Cancer Screening. Academic Radiology 2017;24(2):124-30.
4. Ohno Y, et al. Standard-, Reduced-, and No-Dose Thin-Section Radiologic Examinations: Comparison of Capability for Nodule Detection and Nodule Type Assessment in Patients Suspected of Having Pulmonary Nodules. Radiology 2017;284(2):562-73.
5. Biederer J, et al. Screening for lung cancer: Does MRI have a role? European Journal of Radiology 2017;86:353-60.
6. Bae K, et al. Comparison of lung imaging using three-dimensional ultrashort echo time and zero echo time sequences: preliminary study. European Radiology 2019;29(5):2253-62.
7. Nomura Y, et al. Preliminary study of automated detection of pulmonary nodule in ultrashort echo time MR images. International Journal of Computer Assisted Radiology and Surgery 2019;14(Supplement1):S82-3.
Figures