2291
Hyperpolarized 129Xe MRI Measures of Gas Exchange in Non-specific Interstitial Pneumonia1Radiology, Duke University, Durham, NC, United States, 2Biomedical Engineering, Duke University, Durham, NC, United States, 3Medicine, Duke University, Durham, NC, United States
Synopsis
Hyperpolarized 129Xe gas exchange MRI was used to compare patients with non-specific interstitial pneumonia (NSIP) and healthy controls. NSIP patients had significantly increased interstitial barrier uptake and decreased red blood cell transfer despite preserved ventilation; in some cases, these abnormalities were present without spatially associated CT findings. These results suggest that 129Xe gas exchange MRI is sensitive to disease activity that is not reflected on 129Xe ventilation alone, or on CT. Ongoing analyses will test the ability of this technique to assess response to targeted therapies and guide clinical decision making in NSIP and other interstitial lung diseases.
Introduction
Non-specific interstitial pneumonia (NSIP) is a distinct form of interstitial lung disease (ILD) with a generally good prognosis1. NSIP may be either idiopathic or associated with conditions such a Sjögren’s syndrome, rheumatoid arthritis, and connective tissue disorders. However, a definitive diagnosis requires a comprehensive clinical assessment coupled with CT findings and potential invasive surgical lung biopsy (SLB)1. In caring for patients with NSIP and other ILD’s, a pressing need is emerging to develop techniques suitable for repeated, longitudinal assessment of disease progression and treatment response. This will ensure that individual patients are receiving effective treatment, and prompt the consideration of different or escalated therapy approaches if they are not.Hyperpolarized (HP) 129Xe MRI enables the visualization and quantification of three compartments of gas exchange, namely ventilation, interstitial barrier uptake, and red blood cell (RBC) transfer. While this technique has been applied in idiopathic pulmonary fibrosis (IPF)2-4, further work is needed to better understand its clinical utility across the ILD spectrum. Here, we present the first images of 129Xe gas exchange MRI in patients with NSIP. We compare quantitative measurements of ventilation defect percent, (VDP) mean interstitial barrier tissue signal, and mean RBC signal in NSIP patients vs. healthy volunteers.
Methods
HP 129Xe MRI was acquired in 32 NSIP subjects (9M 23F, 57.0±10.7 yrs) and 18 healthy subjects (14M 4F, 32.8±13.5 yrs). CT was acquired for all NSIP subjects as part of standard clinical care. Subjects inhaled 1L 129Xe/N2 blend from functional residual capacity (FRC) and 3D images were acquired using three interleaved sets of 1000 views of the gas and dissolved compartments (TR = 15 ms, flip angle = 0.5/20°, and TE = TE90). Dissolved-phase (i.e. barrier and RBC) measurements were decomposed using the 1-point Dixon method5. Ventilation, barrier, and RBC images were rendered into quantitative maps using a clustering method based on reference distributions derived from a healthy cohort as described previously2. VDP, mean barrier/gas signal, and mean RBC/gas signal were compared in the NSIP patients vs. healthy subjects using the Wilcoxon rank-sum test.Results
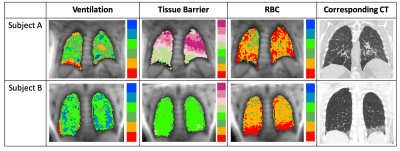
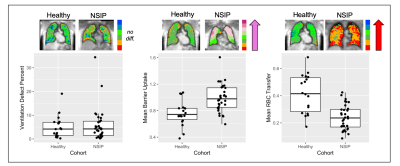
Typical 129Xe MRI and CT images from two NSIP subjects are shown in Figure 1. This pattern of low VDP, normal-to-high barrier signal, and greatly reduced RBC signal was broadly consistent across this study population. As shown in Figure 2, NSIP subjects showed a similar VDP as healthy controls (p = 0.88) but a significantly increased tissue barrier uptake (p < 0.0001) and significantly decreased RBC transfer (p < 0.0001. Figure 2 also depicts instances of prominent bibasilar RBC transfer defects spatially associated with CT findings of structural remodeling. However, RBC deficits were also noted in regions where the corresponding CT is unremarkable.Discussion
These results suggest that ventilation measurements alone are insufficient for assessing ILD’s and highlight the importance of assessing dissolved-phase 129Xe MRI measurements. The qualitative evidence of regional correspondence between 129Xe gas exchange abnormalities and structural remodeling on CT provides evidence that localized disease processes can manifest on both modalities. Moreover, the observation that regions of reduced RBC transfer were also present in the absence of corresponding disease findings on CT suggests that 129Xe imaging may be sensitive to early functional abnormalities that may precede later-stage structural abnormalities detected on CT.Conclusion
HP 129Xe MRI is a viable means of assessing gas exchange abnormalities in NSIP, and the non-ionizing nature of MRI suggests a potential role for repeated 129Xe imaging in longitudinal monitoring of disease progression and therapy response. Ongoing analyses will test the ability of this technique to assess response to targeted therapies, identify imaging-based disease phenotypes, and guide clinical decision making in NSIP and other interstitial lung diseases.Acknowledgements
NIH R01HL105643, R01HL126771References
1Travis et al., Am J Respir Crit Care Med, Vol 177. pp 1338-1347, 2008.
2Wang, JM, Robertson SH, Wang Z, et al. Thorax 2018;73:21-28.
3Mammarappallil JG, et al. J Thorac Imaging 2019;34(2):136-150.
4Rankine LJ et al., American Thoracic Society [In Press.]
5Kaushik et al., MRM, 2016.
Figures