2288
Assessment of Gas Exchange for Lung Volume Reduction Surgery in an Emphysema Rat Model Using Xenon Polarization Transfer Contrast Imaging1Radiology, University of Pennsylvania, Philadelphia, PA, United States, 2Bioengineering, University of Pennsylvania, Philadelphia, PA, United States, 3Surgery, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Lung volume reduction surgery (LVRS) treats emphysema by removing severely emphysematous regions of the lung. Techniques that can better identify which regions of the lung to remove as well as assess the resultant changes in lung function could lead to better surgical outcomes. Here, we explored the feasibility of using hyperpolarized xenon-129 (HXe) MRI for this purpose. Xenon polarization Transfer Contrast (XTC) imaging was used to quantify gas exchange as a metric for assessing the severity and distribution of emphysematous lung regions before and after LVRS.
Introduction
Emphysema is one of the most common forms of chronic lung disease. Assessing its severity and distribution is particularly relevant for lung volume reduction surgery (LVRS), a treatment that involves removing the severely emphysematous lung regions to allow the remaining functional regions to expand. Hyperpolarized xenon-129 (HXe) MRI provides a valuable tool for assessing the changes in lung structure and function associated with this disease. Unfortunately, direct imaging of the dissolved-phase components is challenging due to significantly reduced gas exchange in the case of emphysema, which results in lower SNR. However, Xenon polarization Transfer Contrast (XTC) imaging has the ability to capture gas exchange by imaging gas-phase (GP) signal, which has higher SNR, before and after repeated saturations of either the red blood cell (RBC) or tissue plasma (TP) components1. In this work, we explored XTC’s ability to identify emphysematous regions and assess disease severity.Methods
Imaging was performed in 4 male Wistar rats (300 – 340 g) and approved by the Institutional Animal Care and Use Committee. Emphysema was induced in via localized elastase injections (100 mL/g) approximately one month prior to imaging. Animals were ventilated with room air and then switched to an 80% HXe, 20% oxygen mixture for 4 wash-in breaths, followed by imaging during a 10 second end-inspiratory breath-hold. In one animal, an emphysematic right upper lobe was excised and post-LVRS images were obtained.Three consecutive gas-phase images were acquired for XTC. Parameters for the 2D GRE included: flip angles of 4°, 9°, and 13°, respectively, TR/TE = 7.9/3.8 ms, matrix size = 36x48, and FOV of 65 mm. For coronal images, two 19 mm slices were acquired; projections were acquired for the axial images. Contrast preparation was applied between the second pair of images and consisted of 100 frequency selective Gaussian inversion pulses (width = 8 ms, TR = 30 ms) centered at either 215 ppm (RBC resonance) or 198 ppm (TP resonance). Between the first pair of images, this same contrast preparation scheme was repeated off-resonance (either -215 ppm or -198 ppm) in order to correct for T1 decay and gas-phase magnetization loss due to a combination of the imaging and inversion pulses. Maps of the depolarization per inversion pulse were calculated from the ratios of these images, which are directly related to dissolved-phase (DP)-to-gas-phase (GP) ratios. Apparent diffusion coefficient (ADC) maps were obtained from a hybrid imaging protocol, with b-values of 0 and 16.9 s/cm2 for the diffusion gradients2.
Tidal volumes were determined from CT, and all MR imaging was performed on a 1.5 T scanner (Magnetom Avanto, Siemens) with a custom xenon-129 birdcage coil (Stark Contrast, Germany). A prototype commercial system (XeBox-E10, Xemed LLC, NH) was used to polarize 87% enriched xenon-129.
Results
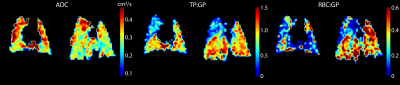
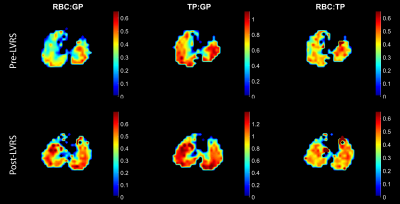
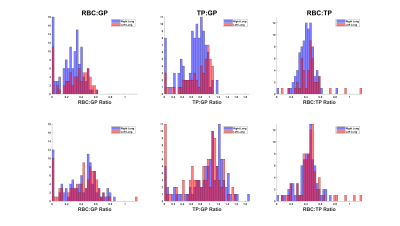
Figure 1 shows a comparison of ADC with both RBC:GP and TP:GP ratios derived from XTC maps for a representative animal. The elevated ADC in the right upper lobe is indicative of emphysema. The TP:GP ratio, in particular, highlights the difference between the emphysematous and healthy tissue; the decrease in TP:GP is consistent with emphysema-associated tissue destruction. This contrast is slightly less apparent in the RBC:GP ratio. Figure 2 shows the RBC:GP, TP:GP, and RBC:TP ratios before and after LVRS, which depict a notable expansion of the left lung. Prior to surgery, the averages of the ratios were 0.28, 0.68, and 0.43, respectively, for RBC:GP, TP:GP, and RBC:TP. After surgery, these increased to 0.4, 0.89, and 0.47. While there was an overall increase in both the RBC:GP and TP:GP values, the RBC:TP ratio remained fairly similar. There was, however, a marked increase of the ratios in the right lung compared to the left lung, as seen in the histograms in figure 3.Conclusion
Frequency selective XTC is capable of identifying emphysematous lung regions which correlate with ADC measurements, and of demonstrating an increase in gas exchange after LVRS.Acknowledgements
No acknowledgement found.References
[1] Ruppert, Kai, et al (2000). Probing lung physiology with xenon polarization transfer contrast (XTC). MRM 44(3), 349-357.
[2] Hamedani, Hooman, et al (2016). Regional fractional ventilation by using multibreath wash-in 3He MR imaging. Radiology 279(3), 917-924.
Figures