2285
Regional hyperpolarised 129-xenon MR spectroscopy and diffusion-weighted MRI in patients with idiopathic pulmonary fibrosis
James A Eaden1,2, Ho-Fung Chan1, Guilhem J Collier1, Nicholas D Weatherley1, Jim Lithgow1, Oliver Rodgers1, Jody FD Bray1, Graham Norquay1, Stephen M Bianchi2, and Jim M Wild1,3
1POLARIS, MRI unit, Department of Infection Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 2Academic Directorate of Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 3Insigneo institute, University of Sheffield, Sheffield, United Kingdom
1POLARIS, MRI unit, Department of Infection Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 2Academic Directorate of Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 3Insigneo institute, University of Sheffield, Sheffield, United Kingdom
Synopsis
Preliminary findings are presented from a prospective, longitudinal hyperpolarised 129Xe MRI study of idiopathic pulmonary fibrosis patients. To date, 28 patients have undergone baseline 129Xe DW-MRI and 10 patients have returned for a six-month scan. 14 patients have undergone baseline dissolved 129Xe imaging using IDEAL CSI method. Regional values were produced by separating the lung into three zones. We demonstrate regional differences in 129Xe gas transfer and 129Xe DW-MRI measurements. LmD was found to be more sensitive to longitudinal change than ADC. Over a six-month period, the significant change in mean 129Xe LmD was observed in the lower zone only.
Introduction
Idiopathic pulmonary fibrosis (IPF) is a progressive lung disease with a poor prognosis. Scarring predominantly affects the lung bases, resulting in a reduction in gas exchange. Pulmonary function tests are relatively insensitive to early change in IPF, thus the need for more sensitive markers of lung structure-function is well recognised1. The proposed study is a prospective, observational study of patients with IPF from a tertiary referral centre.Hyperpolarised 129xenon (129Xe) MR spectroscopy can be used as a quantitative marker of gas exchange and diffusion limitation in IPF. The ratio of the uptake of 129Xe in the red blood cells (RBCs) to the tissue/plasma (TP) barrier (RBC:TP) has been shown to be reduced by 70% in IPF patients when compared with healthy volunteers2. Previous studies found that the decline in RBC:TP in IPF patients over 12 months was not accompanied by a significant change in diffusing capacity of the lung for carbon monoxide (DLCO) or carbon monoxide transfer coefficient (KCO)3.
The apparent diffusion coefficient (ADC) is a measure of Brownian gas diffusion in the airspaces, where restrictions by tissue boundaries provide information about lung microstructure down to the alveolar level. Significant correlation has been found between helium (3He) ADC and 129Xe ADC4. The mean diffusive length scale (LmD), is a diffusion weighted (DW) MRI lung microstructure measurement calculated using a stretched exponential fit method. DW-MRI with hyperpolarised 3He in IPF patients has demonstrated that ADC and LmD correlates with DLCO, KCO and regional fibrosis on CT5. In the same study, there was no significant change in ADC, however, LmD increased significantly over 12-months5. To date, no data are available on the utility of 129Xe diffusion in IPF.
Methods
To date, 28 patients have undergone baseline 129Xe DW-MRI and 10 patients have returned for a six-month follow-up scan. Additionally, 14 patients have undergone baseline dissolved 129Xe imaging. Imaging was performed on a 1.5T GE HDx scanner. 129Xe was polarised by spin-exchange optical pumping6.A 3D multiple b-value DW-MRI sequence (b=0, 12, 20, 30 s/cm2) was acquired and maps of ADC and LmD were calculated from 129Xe DW-MRI for each imaging voxel using a mono-exponential fit of the first two DW b-values (b=0, 12 s/cm2)7. 550mL of 129Xe was mixed with nitrogen to balance a total inhaled dose of 1L.
MR imaging of 129Xe gas/dissolved compartments used the IDEAL method of water-fat separation applied previously for 13C metabolic imaging8 and a 1L dose of pure hyperpolarised 129Xe. A 3D radial flyback k-space trajectory (4 TE per TR) SPGR sequence with an alternative and separate RF excitation of gaseous and dissolved-phase 129Xe (FA=0.6/400, respectively) was implemented (332 projections, 2cm isotropic resolution, FOV=40cm, BW=31.25kHz, TR=20ms, 14s acquisition time during breath-hold). A spectroscopic calibration scan (BW=8kHz, 512pts, 200 averages, TR=74ms, 220 flip angle) was performed prior to imaging to improve reconstruction.
Regional RBC:TP and DW-MRI values were produced by separating the lung into three zones (upper, middle and lower). Friedman test was used to determine statistical differences between the three lung zones. Paired t-test was used to determine statistical differences between study visits. Pearson correlation coefficient was used to determine the strength of correlations. Significance was assumed at p<0.05.
Results
At baseline, a significant difference in 129Xe RBC:TP was found between the lower and middle zones (p=0.049), middle and upper zones (p=0.0018), and lower and upper zones (p=0.0063) (Figure 1). A significant difference in mean 129Xe ADC was seen between the middle and upper zones (p<0.001) but not between the lower and middle zones (p=0.098) or the lower and upper zones (p=0.37) (Figure 2a-b). Similarly, a significant difference in mean 129Xe LmD was observed between the middle and upper zones (p=0.0099) but not between the lower and middle zones (p=0.86) or the lower and upper zones (p=0.18) (Figure 2c-d).There was no significant longitudinal change in mean 129Xe ADC for each of the three lung zones (Figure 3). However, there was a significant longitudinal change in mean 129Xe LmD in the lower zone (p=0.044) but not the middle zone (p=0.076) or upper zone (p=0.24) (Figure 4).
A significant correlation was found between 129Xe RBC:TP and mean 129Xe ADC in the upper zone (r=0.56; p=0.036) but no correlation was seen between 129Xe RBC:TP and mean 129Xe ADC in the lower zone or middle zone (Figure 5a-c). No significant correlation was observed between 129Xe RBC:TP and mean 129Xe LmD in any of the three lung zones (Figure 5d-f).
Discussion
Our preliminary findings demonstrate regional differences in both 129Xe RBC:TP and 129Xe DW-MRI measurements in IPF patients. 129Xe LmD was found to be more sensitive to longitudinal change than 129Xe ADC which is in keeping with the 3He DW-MRI findings previously reported5. Over a six-month period, the significant change in 129Xe LmD was observed in the lower zone only which is to be expected given that IPF is a disease that predominantly affects the lung bases. However, statistically significant differences in 129Xe ADC and LmD were found only between the middle and upper zones at baseline scan. It is possible that the middle zones are affected by IPF, even where the macroscopic structure of the lung is normal.Acknowledgements
Study supported by Boehringer Ingelheim, National Institute for Health Research (NIHR-RP-R3-12-027) and the Medical Research Council (MR/M008894/1). The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research or the Department of Health.References
- Wild JM. Imaging pathophysiological changes in the lungs in IPF with xenon magnetic resonance imaging. Thorax. 2018; 73:1.
- Kaushik SS, Freeman MS, Yoon SW, et al. Measuring diffusion limitation with a perfusion limited gas – Hyperpolarized 129Xe gas-transfer spectroscopy in patients with idiopathic pulmonary fibrosis. J Appl Physiol. 2014; 117:577-585.
- Weatherely ND, Stewart NJ, Chan H-F, et al. Hyperpolarised xenon magnetic resonance spectroscopy for the longitudinal assessment of changes in gas diffusion in IPF. Thorax. 2019; 74:500-502.
- Kirby M, Svenningsen S, Owrangi A, et al. Hyperpolarized 3He and 129Xe MR imaging in healthy volunteers and patients with chronic obstructive pulmonary disease. Radiology. 2012; 265:600-610.
- Chan H-F, Weatherley ND, Johns CS, et al. Airway Microstructure in Idiopathic Pulmonary Fibrosis: Assessment at Hyperpolarized 3He Diffusion-weighted MRI. Radiology. 2019; 291:223-229.
- Norquay G, Collier GJ, Rao M, et al. 129Xe-Rb spin-exchange optical pumping with high photon efficiency. Phys. Rev. Lett. 2018; 121:153201.
- Chan HF, Stewart NJ, Norquay G, et al. 3D Diffusion-Weighted 129Xe MRI for Whole Lung Morphometry. Magn Reson Med, 2018; 79:2986–2995.
- Wiesinger F, Weidl E, Menzel MI, et al. IDEAL spiral CSI for dynamic metabolic MR imaging of hyperpolarized [1-13C] pyruvate. Magn Reson Med. 2012; 68(1):8-16.
Figures
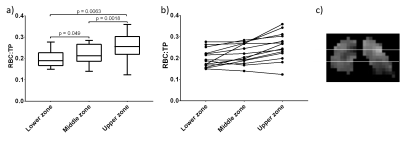
Figure 1. Difference in 129Xe RBC:TP between the lower, middle and upper zones at baseline
visit (a-b) (n=14). Example of a 129Xe
RBC:TP image separated into lower, middle and upper zones (c).
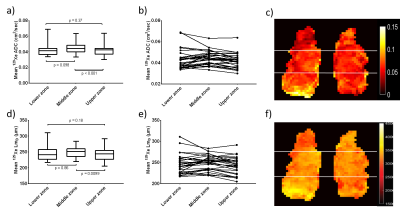
Figure 2. Difference in mean
129Xe ADC (a-b) and mean 129Xe LmD (d-e) between the
lower, middle and upper zones at baseline visit (n=28). Example of a mean 129Xe ADC image (c) and a mean 129Xe LmD image (f) separated into lower, middle and
upper zones.
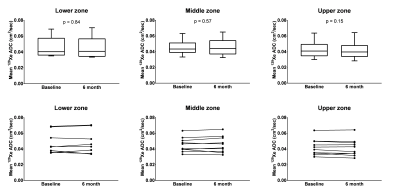
Figure 3. Longitudinal change in mean 129Xe ADC for each of the three lung zones (n=10).
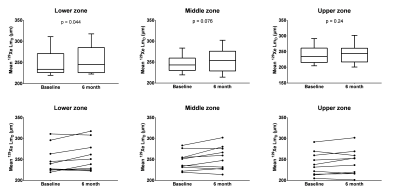
Figure 4. Longitudinal change in mean 129Xe LmD
for each of the three lung zones (n=10).
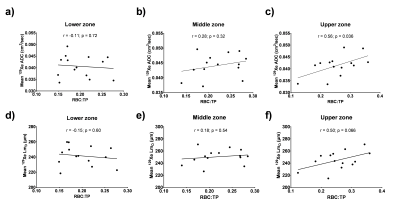
Figure 5.
Correlation between 129Xe
RBC:TP and mean 129Xe ADC for each of the three lung zones (a-c), and
correlation between 129Xe
RBC:TP and mean 129Xe LmD
for each of the three lung zones (d-f) (n=14).