2283
Noninvasive Diagnosis of Pulmonary Hypertension with Hyperpolarized 129Xe Magnetic Resonance Imaging and Spectroscopy1Biomedical Engineering, Duke University, Durham, NC, United States, 2Radiology, Duke University Medical Center, Durham, NC, United States, 3Medical Physics Graduate Program, Duke University, Durham, NC, United States, 4Division of Cardiology, Department of Medicine, Duke University Medical Center, Durham, NC, United States
Synopsis
Using unique signatures in 129Xe MR 3D gas exchange imaging and dynamic spectroscopy, we tested an algorithm to detect pulmonary hypertension (PH). The algorithm was developed using a training cohort (n=105) and tested on 25 subjects whose PH status was determined via right heart catheterization. Two expert readers rated scan quality and interpreted each subject’s 129Xe MRI/MRS to determine PH status. Using the 16 patients for which readers rated scan diagnostic quality as 4-5/5, the diagnostic accuracy was 0.84 (sensitivity=0.78, specificity=0.93). This model demonstrates the ability to distinguish subjects with pre-capillary PH from those without PH or with post-capillary PH.
Purpose:
Pulmonary arterial hypertension (PAH) is a form of pulmonary vascular disease (PVD) characterized by pulmonary hypertension (PH – an elevated blood pressure in the lungs) that results in progressive right ventricular (RV) failure. Diagnosis of PAH requires meeting specific right heart catheterization (RHC) hemodynamic criteria. However, this technique is invasive and can be difficult to interpret in patients with other cardiopulmonary disease that may cause PH. In those patients, PAH therapies are contra-indicated. Hence, it is critical to develop non-invasive methods to detect PH and determine whether it is pre- or post-capillary. Recent work has demonstrated that hyperpolarized 129Xe MR gas exchange imaging and spectroscopy exhibit unique patterns associated with various cardiopulmonary diseases, including (PAH), chronic obstructive pulmonary disease (COPD), and interstitial lung disease (ILD)1. Here we sought to use these signatures to develop a diagnostic algorithm to detect PH and classify if it is pre-capillary PH (PAH).Methods:
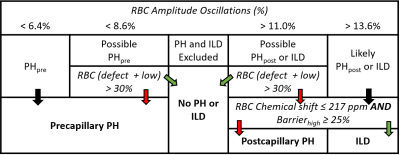
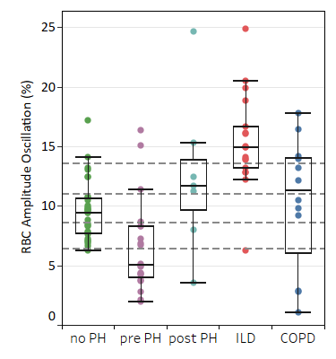
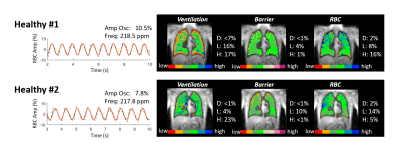
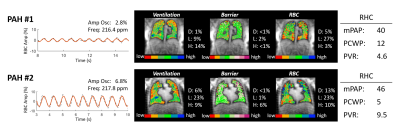
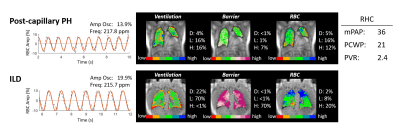
All subjects underwent 3D 129Xe gas exchange MRI2 and dynamic spectroscopy (TR=20ms)3. Gas exchange images were transformed into quantitative maps depicting ventilation, barrier tissue uptake, and red blood cell (RBC) transfer4. Each compartment was binned and quantified by its defect, low, and high percentage. The dynamic spectroscopy was used to determine the cardiogenic RBC amplitude variation, while static analysis determined the RBC frequency shift. A training cohort of 105 subjects (no PH n=38, pre-capillary PH n=22, post-capillary PH n=9, ILD n=24, COPD n=12) was used to construct a diagnostic algorithm. The required tests and detection thresholds were determined using receiver operating characteristic (ROC) curves and a decision-tree machine-learning algorithm. The resulting algorithm (Figure 1) first uses the RBC signal oscillation amplitude (Figure 2) to determine presence of PH and, if so, whether it is pre- or post-capillary. For equivocal cases, the additional presence of large regions (>30%) of defect/low RBC transfer confirms PH on both the pre- and post-capillary branches. Differentiation of ILD from post-capillary PH required testing for presence of enhanced barrier uptake (>25%) and low RBC shift (<217 ppm). The algorithm was tested using a cohort of 25 patients examined by 129Xe MRI/MRS, for whom RHC was also performed on the same day (n=16) or within 2 months (n=9). RHC measurements of mean pulmonary artery pressure (mPAP), pulmonary capillary wedge pressure (PCWP), and pulmonary vascular resistance (PVR) were used to determine PH status (no PH, pre-capillary, post-capillary, or combined pre- and post-capillary PH (CpcPH)). A diagnosis of PH was established from mPAP≥20mmHg, while PAH required PCWP≤15mmHg, and PVR≥3 Woods Units5. Patient with high PVR and PCWP>15mmHg were classified as CpcPH. Two expert readers (cardiothoracic radiologists), blinded to the RHC findings, were trained to interpret 129Xe MRI/MRS and apply the diagnostic algorithm. They were asked to rate the diagnostic quality of the scans for each subject, and determine if the subject had PH, and whether it was pre-capillary.Results:
In 25 test subjects, RHC indicated 12 subjects had pre-capillary PH only, while 3 had CpcPH. The readers agreed on all but 1 classification of pre-capillary PH. Without considering MRI/MRS quality, the baseline diagnostic accuracy was 0.7 with a sensitivity of 0.6, and a specificity of 0.85. However, in the 16 test subjects rated as having good diagnostic quality (4 or 5 out of 5), diagnostic accuracy increased to 0.87 (sensitivity=0.88, specificity=0.86). Readers also identified 13 subjects (8 with pre-capillary PH) as having other extensive lung disease (either COPD or ILD).Discussion:
Without considering MRI/MRS scan quality, the model had a modest accuracy. However, the majority of misclassified subjects were attributable to spectroscopic SNR. After excluding low SNR cases, the only misclassified subjects were a subject with CpcPH predicted to have no PH, and a subject with chronic thromboembolic pulmonary hypertension (CTEPH) classified as having pre-capillary PH, when RHC did not. Out of the 3 subjects with CpcPH, including those with low diagnostic quality, readers only classified 1 with pre-capillary PH. Classification of CpcPH is challenging because RBC amplitude thresholds for pre- and post-capillary PH are mutually exclusive. In pure pre-capillary PH RBC amplitude oscillations are suppressed while in pure post-capillary PH, they are enhanced. In CpcPH these two effects likely cancel to yield RBC amplitude oscillations in the healthy reference range. It may be feasible to better discriminate this condition by imaging RBC oscillations, as recently demonstrated. The misclassification of the CTEPH patient by 129Xe MRI may be an artifact of RHC. CTEPH is considered a form of pre-capillary PH, although post-capillary vascular remodeling has been noted. This patient had a PVR of 2.8 Woods Units mmHg, close to the threshold for pre-capillary PH and thus classified by RHC as neither post-capillary nor pre-capillary. We should note that future work may significantly improve diagnostic accuracy by not only focusing on obtaining RBC dynamics with high SNR, but also adding a limited cardiac MRI exam to measure the stroke volume that, in conjunction with vascular impedances, affects the RBC amplitude oscillations.Conclusion:
The proof-of-concept diagnostic model demonstrates the potential of 129Xe MRI/MRS to non-invasively distinguish subjects with pre-capillary PH from patients with no PH or post-capillary PH. With further optimization it will be positioned for testing in larger, multicenter studies.Acknowledgements
This work was supported by the NIH (R01HL126771 and HHSN268201700001C).
References
1. Wang Z, Bier EA, Swaminathan A, Parikh K, Nouls J, He M, Mammarappallil JG, Luo S, Driehuys B, Rajagopal S. Diverse Cardiopulmonary Diseases are Associated with Distinct Xenon MRI Signatures. European Respiratory Journal 2019.
2. Kaushik SS, Robertson SH, Freeman MS, He M, Kelly KT, Roos JE, Rackley CR, Foster WM, McAdams HP, Driehuys B. Single-breath clinical imaging of hyperpolarized 129xe in the airspaces, barrier, and red blood cells using an interleaved 3D radial 1-point Dixon acquisition. Magnetic Resonance in Medicine 2016;75(4):1434-1443.
3. Bier EA, Robertson SH, Schrank GM, Rackley C, Mammarappallil JG, Rajagopal S, McAdams HP, Driehuys B. A protocol for quantifying cardiogenic oscillations in dynamic 129Xe gas exchange spectroscopy: The effects of idiopathic pulmonary fibrosis. NMR in Biomedicine 2019;32(1):e4029.
4. Wang Z, Robertson SH, Wang J, He M, Virgincar RS, Schrank GM, Bier EA, Rajagopal S, Huang YC, O'Riordan TG. Quantitative Analysis of Hyperpolarized 129Xe Gas Transfer MRI. Medical Physics 2017.
5. Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, Sanchez MAG, Kumar RK, Landzberg M, Machado RF. Updated clinical classification of pulmonary hypertension. Journal of the American College of Cardiology 2013;62(25 Supplement):D34-D41.
Figures