2281
Discrete Wavelet Transform (DWT) Denoising of Hyperpolarized 129Xe MR Images1Imaging Research Centre, St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada, 2Department of Electrical and Computer Engineering, McMaster University, Hamilton, ON, Canada, 3Department of Medicine, McMaster University, Hamilton, ON, Canada, 4Firestone Institute for Respiratory Health, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada
Synopsis
Hyperpolarized 129Xe MRI is an attractive approach to regionally quantify ventilation, however, it often suffers from low SNR. The use of a wavelet transform algorithm was explored as a way to improve SNR while not compromising image detail. Various wavelets and sparsity parameters were explored, all of which provided a significant improvement in SNR while minimally impacting image detail.
Introduction
The use of hyperpolarized 129Xe MRI to non-invasively visualize and quantify lung ventilation in pulmonary disease is well established.1 However, signal-to-noise ratio (SNR) remains a challenge, especially for sites with older generation polarizers that achieve <20% 129Xe polarization. Even sites with state-of-the-art polarizers that produce >30% polarization may wish to reduce the amount of hyperpolarized 129Xe delivered, thus reducing cost and production time, and accept lower SNR. The principle behind the wavelet transform is to transpose data into a representation that concentrates important features into a few wavelet coefficients, thus allowing application of a threshold to reduce unwanted coefficients (i.e. noise). Our objective was to explore the use of the discrete wavelet transform (DWT) for improving SNR of low polarization (<12%) 129Xe lung MR images without compromising fine detail structures that may be relevant to underlying lung anatomy and pathology.Methods
Subjects: Inhaled hyperpolarized 129Xe lung MR images from 14 subjects (6 males, 8 females; mean age 39 years, range 20-62 years, 6 healthy, 8 patients with asthma) acquired at the Firestone Institute for Respiratory Health (Hamilton, Canada) were used to test the wavelet denoising algorithm. All subjects provided written informed consent to an ethics-board approved protocol.Image Acquisition: Images were acquired on a 3.0 Tesla MRI (Discovery MR750, General Electric Healthcare, Milwaukee, USA) using a home-built asymmetric quadrature birdcage 129Xe coil.2 Hyperpolarized 129Xe gas was provided by a turn-key, spin-exchange polarizer (Polarean 9800, polarization range: 7-11%). Polarization was measured using a polarization measurement station (Polarean Inc., Durham, USA) and the dose equivalent (DE) volume of 100% enriched, 100% polarized 129Xe was calculated.3 129Xe ventilation images were acquired using a 3D fast gradient-echo pulse sequence (3.1x3.1x15mm resolution, 16 slices, 11 second scan time) as previously described4 in breath-hold after inspiration of 1.0L of 129Xe/N2 mixture from functional residual capacity.
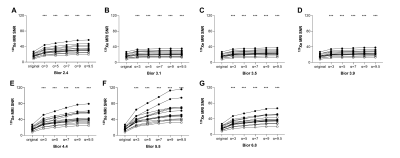
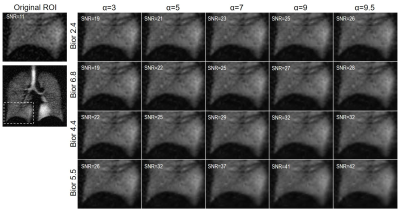
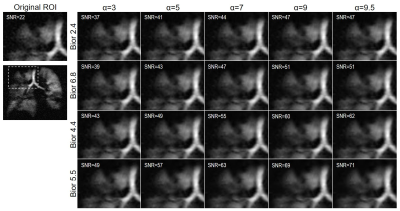
Image Processing: An image filtering algorithm, utilizing the biorthogonal wavelet transform (bior), was developed using the wavelet toolbox in Matlab (MathWorks Inc, Natick, USA). The biorthogonal mother wavelet was selected because it was designed for image denoising, while preserving structure. The following variations were tested: bior2.4, bior3.1, bior3.5, bior3.9, bior4.4, bior5.5 and bior6.8. The sparsity parameter, α, which determines the noise threshold, was varied between 3 and 9.5, resulting in 35 different wavelet denoised images per subject. A single central slice including the trachea and main bronchi from each subject was used to evaluate the denoising effect of various wavelet transforms.
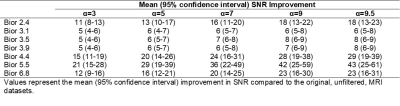
Data Analysis and Statistics: The SNR of the original, unfiltered, datasets were compared to that of the wavelet filtered datasets. SNR was calculated as the mean signal in a region of interest within the ventilated lung, divided by the standard deviation of the background (unstructured) noise in a ROI of the same size outside the lung. For each wavelet transform, a one-way repeated measures ANOVA with the Geisser-Greenhouse correction was performed to compare the SNR of original and denoised MRI datasets. Tukey's multiple comparisons tests were performed to compare the SNR of the original dataset to each denoised MRI dataset. All statistics were performed using GraphPad Prism version 8.1.1 (La Jolla, USA).
Results
The mean dose-equivalent volume of hyperpolarized 129Xe administered was 48±6 mL (minimum of 35, maximum of 56) and the mean SNR of the original, unfiltered, datasets was 17±5 (minimum of 8, maximum of 27). SNR was correlated with the dose-equivalent volume of 129Xe administered to the subject (r=0.61, p=0.02). Figure 1 shows the SNR measured for all wavelet denoised datasets, and Table 1 summarizes the mean SNR improvement. SNR was significantly improved for all wavelet transforms and α combinations (bior2.4, p<0.0001; bior3.1, p<0.0001; bior3.5, p<0.0001; bior3.9, p<0.0001; bior4.4, p<0.0001; bior5.5, p<0.0001; bior6.8, p<0.0001). The greatest SNR improvement was observed using the bior5.5 wavelet with an α=9.5 (mean SNR increase of 43 (95% CI, 25 to 61), p<0.0001). Whereas the smallest SNR improvement was observed using the bior3.1 (mean SNR increase of 5 (95% CI, 4 to 6), p<0.0001), bior3.5 (mean SNR increase of 5 (95% CI, 4 to 6), p<0.0001) and bior3.9 (mean SNR increase of 5 (95% CI, 4 to 6), p<0.0001) wavelets with a α=3. Representative original and denoised 129Xe MR images are shown for a healthy volunteer and patient with severe asthma in Figure 2 and 3, respectively. Across all wavelet transforms, as α increased, there is an increasing smoothness in the denoised images. Importantly, fine details including vasculature voids and ventilation defect boundaries were well-preserved in the denoised images.Discussion
The use of the DWT significantly improved SNR of low polarization 129Xe MR images. Importantly, fine structures such as vascular voids and ventilation defect boundaries, were well-preserved. It is anticipated that ventilation defect computations, which are sensitive to noise, will see improvements in speed and accuracy with the use of a DWT precursor. The observed image smoothing requires further exploration with image texture analysis, and understanding with respect to modulation of image point spread function.Conclusions
The biorthogonal wavelet transform is an effective tool to improve the SNR of hyperpolarized 129Xe MRI. Significantly improved SNR was observed even at modest noise thresholds, while fine structures were preserved across all thresholds and wavelets tested.Acknowledgements
The authors thank M. Kjarsgaard and C. Huang for helping with recruitment and assessment of study subjects, and J. Lecomte, C. Awde, T. DiLeonardo and S. Faseruk, the MRI technologists who performed the scanning.
References
1. Ebner L, Kammerman J, Driehuys B, et al. The role of hyperpolarized 129Xe in MR imaging of pulmonary function. Eur J Radiol. 2017;86:343-352.
2. Farag A, Wang J, Ouriadov A, et al. Unshielded and asymmetric RF transmit coil for hyperpolarized 129Xe human lung imaging at 3.0 T. Proc Intl Soc Mag Reson Med. 2012.
3. He MS, Robertson SH, Suryanarayanan SK, et al. Dose and pulse sequence considerations for hyperpolarized 129Xe ventilation MRI. Magn Reson Imaging. 2015;33(7):877-885.
4. Svenningsen S, Kirby M, Starr D, et al.
Hyperpolarized 3He and 129Xe MRI: differences in asthma before
bronchodilation. J Magn Reson Imaging. 2013;38(6):1521-1530.
Figures