2277
Noninvasive Pressure Measurements in the Transverse Sinuses using ICOSA6 4DFlow – an In Vitro Validation with Catheter-based Manometry1University of California, San Francisco, San Francisco, CA, United States, 2Siemens Healthcare, Chicago, IL, United States, 3Siemens Healthcare, San Francisco, CA, United States, 4Veterans Affairs Medical Center, San Francisco, CA, United States
Synopsis
Idiopathic intracranial hypertension is a condition of elevated intracranial cerebrospinal fluid pressure. Transverse sinus stenoses are clearly related to the pathophysiology, and catheter-based manometry is the “gold standard” to assess pressure gradients across these stenoses. The aim of this work is to evaluate the feasibility of assessing these pressure gradients in the intracranial veins using 4DFlow with ICOSA6 motion encoding – which also account for turbulence - and to compare these pressure gradients with catheter-based manometry. Pressure gradient were measured in patient specific phantoms using both 4DFlow and catheter-based manometry. The pressure gradient assessed showed good agreement when accounting for turbulence.
Introduction
Idiopathic Intracranial Hypertension (IIH) is a condition of elevated intracranial cerebrospinal fluid (CSF) pressure and is associated with irreversible vision loss, severe headaches, and pulsatile tinnitus1. Bilateral transverse sinus stenoses are clearly related to the pathophysiology. While the inciting event of IIH is unknown, it is apparent that transverse sinus stenoses are a critical part of a positive feedback loop, and disrupting transverse sinus stenoses with venous sinus stenting can break the vicious cycle and cure IIH and the associated pulsatile tinnitus2–9. The pressure gradient across a stenosis is a measure of its hemodynamical burden, and assessment of intracranial venous pressure gradients using catheter-based manometry is therefore invaluable in the investigation of IIH.Pressure gradients can be derived from the velocity field obtained with 4DFlow MRI10,11 but has up until recently been unable to account for the turbulence commonly caused by the stenoses with the conventional 4-point velocity encoding. Recently, 4DFlow with ICOSA6 motion encoding has been developed to improve the assessment of pressure gradient measurements across a stenosis taking into account for the turbulence12,13.
The aim of this work is to evaluate the feasibility of assessing pressure gradients in the intracranial veins using 4DFlow with ICOSA6 motion, and to compare these pressure gradients with catheter-based manometry.
Methods
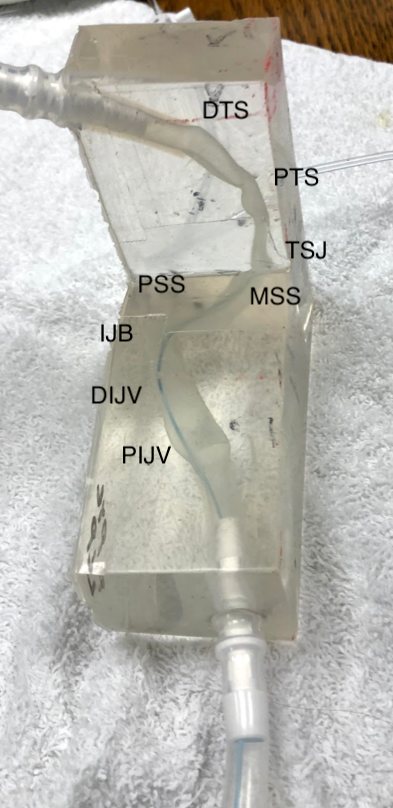
Three patients with IIH underwent MR angiography and lumbar puncture. The intracranial veins were segmented and contoured - from the distal transverse sinus to the proximal internal jugular vein. The geometries were 3D printed in wax using a Solidscape 3Z Max2 3D printer. The printed geometries were cast in Sylgard 184 Silicone, after which the wax was melted away (see Figure 1).Blood mimicking fluid (60% water and 40% glycerol, doped with 10cc Gd-DTPA per 6 liters fluid) was pumped through the patient specific phantoms at 7ml/s. Velocities and turbulence were measured using an ICOSA6 motion encoded 4DFlow sequence using a FOV 160×112×64mm, matrix 320×320×128, TR=8.9ms, TE=5.7ms, flip angle 20°, and VENC=1.5m/s.
The velocities and turbulence (Reynolds stresses) were obtained from the prototype ICOSA6 motion encoded 4DFlow sequence on a clinical 3T scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany), and the pressure gradients were computed by solving the pressure Poisson equation12 – once accounting for the turbulence, and once neglecting the turbulence. Pressure profiles along the veins were generated by extracting the pressure along the centerline of the vessel.
The manometry acquisition was performed using GE Carescape monitor B650. A Codman Prowler Select Plus 0.21” catheter (Codman Neurovascular) was inserted through a 5F access port into extension tubing proximal to the jugular portion of the phantom and navigated into the distal transverse sinus over a guidewire (Boston Scientific Transend EX Guidewire 0.014 in. x 205 cm). Per our clinical protocol pressures are acquired at multiple location along the venous anatomy using a pullback technique. Eight of these location lays within the coverage of the phantoms. The in vitro pressures were therefor assessed using the same technique at these eight discrete locations: Distal Transverse Sinus, Proximal Transverse Sinus, Transverse Sigmoid Junction, Mid Sigmoid Sinus, Proximal Sigmoid Sinus, Internal Jugular Bulb, Distal Internal Jugular Vein, and Proximal Internal Jugular Vein. The catheter-based pressure measurement experiments were repeated three times and values were averaged at each point.
The agreement between pressures obtain by 4DFlow and manometry was evaluated by comparing the total pressure loss across the geometry, as well as the least square error for all eight locations.
Results
The pressure gradient assessed with 4DFlow were in good agreement with the catheter-based manometry for all three geometries when accounting for turbulence using the ICOSA6 technique, as shown in Figure 2 and Table 1. Good agreement was also seen for the non-stenotic phantoms while neglecting the turbulence; however, the deviation increases with increased turbulence generated in the models with a stenosis.Discussion
4DFlow with ICOSA6 motion encoding is able to quantify pressure gradients within the intracranial veins even in the presence of a tight stenosis when compared to catheter-based manometry. ICOSA6 improves accuracy over traditional MR techniques because it accounts for the full effects of pressure loss induced by turbulence energy dissipation. Neglecting the turbulence greatly underestimates the pressure gradient in the stenotic geometry.Conclusion
4DFlow show the potential to accurately assess pressure gradients in the narrow intracranial vessels, even in the presence of a stenosis that causes turbulence.Acknowledgements
No acknowledgement found.References
1. Dinkin MJ, Patsalides A. Venous Sinus Stenting for Idiopathic Intracranial Hypertension: Where Are We Now? Neurol Clin. 2017;35(1):59-81. doi:10.1016/j.ncl.2016.08.006
2. Corbett JJ, Mehta MP. Cerebrospinal fluid pressure in normal obese subjects and patients with pseudotumor cerebri. Neurology. 1983;33(10):1386-1388.
3. Baryshnik DB, Farb RI. Changes in the appearance of venous sinuses after treatment of disordered intracranial pressure. Neurology. 2004;62(8):1445-1446.
4. Scoffings DJ, Pickard JD, Higgins JNP. Resolution of transverse sinus stenoses immediately after CSF withdrawal in idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry. 2007;78(8):911-912. doi:10.1136/jnnp.2006.111765
5. Ahmed R, Friedman DI, Halmagyi GM. Stenting of the transverse sinuses in idiopathic intracranial hypertension. J Neuro-Ophthalmol Off J North Am Neuro-Ophthalmol Soc. 2011;31(4):374-380. doi:10.1097/WNO.0b013e318237eb73
6. Ahmed RM, Wilkinson M, Parker GD, et al. Transverse Sinus Stenting for Idiopathic Intracranial Hypertension: A Review of 52 Patients and of Model Predictions. Am J Neuroradiol. 2011;32(8):1408-1414. doi:10.3174/ajnr.A2575
7. Onder H, Gocmen R, Gursoy-Ozdemir Y. Reversible transverse sinus collapse in a patient with idiopathic intracranial hypertension. BMJ Case Rep. 2015;2015. doi:10.1136/bcr-2014-011606
8. Satti SR, Leishangthem L, Chaudry MI. Meta-Analysis of CSF Diversion Procedures and Dural Venous Sinus Stenting in the Setting of Medically Refractory Idiopathic Intracranial Hypertension. AJNR Am J Neuroradiol. 2015;36(10):1899-1904. doi:10.3174/ajnr.A4377
9. Peng K-P, Fuh J-L, Wang S-J. High-pressure headaches: idiopathic intracranial hypertension and its mimics. Nat Rev Neurol. 2012;8(12):700-710. doi:10.1038/nrneurol.2012.223
10. Tyszka JM, Laidlaw DH, Asa JW, Silverman JM. Three-dimensional, time-resolved (4D) relative pressure mapping using magnetic resonance imaging. J Magn Reson Imaging JMRI. 2000;12(2):321-329.
11. Ebbers T, Wigström L, Bolger AF, Engvall J, Karlsson M. Estimation of relative cardiovascular pressures using time-resolved three-dimensional phase contrast MRI: 3D Relative Cardiovascular Pressures. Magn Reson Med. 2001;45(5):872-879. doi:10.1002/mrm.1116
12. Haraldsson H, Kefayati S, Ahn S, et al. Assessment of Reynolds stress components and turbulent pressure loss using 4D flow MRI with extended motion encoding. Magn Reson Med. 2018;79(4):1962-1971. doi:10.1002/mrm.26853
13. Ha H, Lantz J, Ziegler M, et al. Estimating the irreversible pressure drop across a stenosis by quantifying turbulence production using 4D Flow MRI. Sci Rep. 2017;7:46618. doi:10.1038/srep46618
Figures