2219
Association between intracranial internal carotid artery steno-occlusive disease and diffuse wall thickening in its petrous segment1Renji Hospital, Shanghai Jiaotong University, Shanghai, China, 2Beijing Geriatric Hospital, Beijing, China, 3Aerospace Center Hospital, Beijing, China, 4Siemens Healthcare, Shanghai, China, 5Biomedical Engineering & Center for Biomedical Imaging Research, Tsinghua University, Beijing, China
Synopsis
This study employed isotropic high-resolution SPACE or VISTA sequence to explore the association between intracranial ICA steno-occlusive disease caused by atherosclerosis and diffuse wall thickening (DWT) in ipsilateral petrous ICA. The results indicated that the diffuse wall thickening of petrous ICA is commonly seen among patients with steno-occlusive disease causing by atherosclerotic plaque in intracranial ICA, especially in occluded intracranial ICA.
Introduction
Severe carotid artery stenosis or occlusion may not only lead to ischemia in cerebral parenchyma but also decrease the blood supply to the downstream arterial vessel wall[1]. The deficits of blood supply of vessel wall may activate a series of pathophysiological processes, including endothelial dysfunction and inflammation, and subsequently result in diffuse wall thickening (DWT). Recently, 3D MR vessel wall imaging techniques, such as blood suppressed T1-weighted imaging SPACE (sampling perfection with application-optimized contrast by using different flip angle evolutions) or VISTA (volumetric isotropic turbo spin echo acquisition) have been proposed to evaluate the vessel wall diseases in more vascular segments benefiting from excellent blood suppression and large longitudinal coverage[2]. Previous literatures have shown that patients with steno-occlusive disease in proximal internal carotid artery (ICA) regardless of Moyamoya disease or atherosclerosis, especially in occluded proximal ICA were more likely to have DWT of petrous ICA[3, 4]. The patients without plaque in proximal ICA or vascular inflammatory disease but with plaque in intracranial ICA are commonly found to coexist the DWT in clinical settings. This study sought to investigate the association between intracranial ICA steno-occlusive disease caused by atherosclerosis and DWT in ipsilateral petrous ICA using 3D T1 black blood imaging.Methods
Subjects: A total of 55 patients who were diagnosed with atherosclerosis plaque in intracranial ICA by 3D-SPACE (VISTA) were recruited in this study. 46 patients had unilateral and 9 had bilateral lesions in intracranial ICA. The main exclusion criteria included the following conditions: (1) with steno-occlusive disease in proximal ICA; (2) with vascular inflammatory disease. MR Imaging: 3D head-neck combined vessel wall imaging was performed on two 3T whole-body MR scanner (MAGNETOM Skyra, SIEMENS Healthcare, Erlangen, Germany, or Ingenia, Philips Medical Systems, the Netherlands) with a head coil and a dedicated surface neck coil. The carotid arteries were imaged with 3D T1-SPACE (VISTA) with the following parameters: TR/TE 800/19ms, flip angle 90°, field of view (FOV) 200×180×40mm3, voxel size 0.5×0.5×0.5mm3, blood suppress function was enabled. Image Analysis: All 3D T1-SPACE (VISTA) images were reconstructed with multi-planar reformation (MPR) for measuring luminal stenosis of intracranial ICA. The degree of stenosis of intracranial ICA was classified into the following four categories according to the NASCET (North American Symptomatic Carotid Endarterectomy Trial) criteria: 1-49%, 50-69%, 70-99%, and 100% (total occlusion). The wall thickness of petrous ICAs was measured at the proximal, middle, and distal segments. The average value of these three segments was taken for further analysis. DWT was identified as the mean wall thickness>1.5mm and divided into two categories: mild DWT, thickness<2mm; and severe DWT, thickness≥2mm.Results
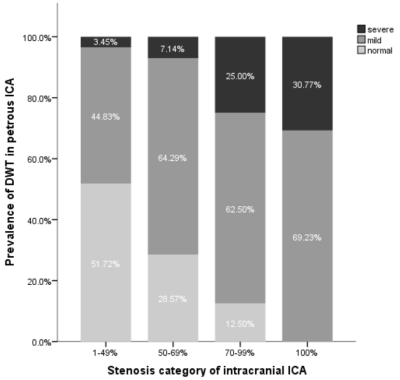
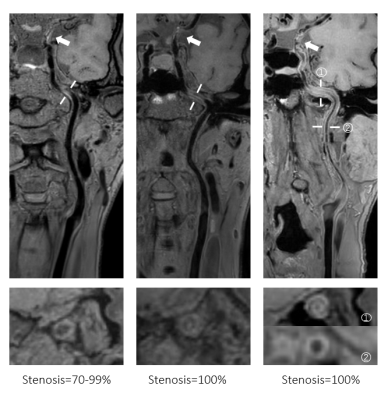
A total of 64 carotid arteries with the steno-occlusive disease in intracranial ICA were included in this study. 29 (45.3%) had 1-49% stenosis, 14 (21.9%) had 50-69% stenosis, 8 (12.5%) had 70-99% stenosis and 13 (20.3%) were diagnosed as total occlusion. Of the 64 ipsilateral petrous ICAs, 20 (31.3%) were normal wall, 36 (56.3%) appeared mild DWT and 8 (12.5%) showed severe DWT according to 3D T1-SPACE (VISTA) images. In the category of 1-49%, 50-69%, 70-99% and total occlusion, the prevalence of severe DWT in petrous ICA was 3.45%, 7.14%, 25.00%, and 30.77%, respectively (Figure 1). No normal wall in petrous ICA was found in arteries with intracranial ICA occlusion. The results also show that 5 arteries of 13 occluded intracranial ICA had DWT not only limited to petrous segment but spread to cervical segment.Discussion and Conclusion
This study found that stenosis in intracranial ICA was obviously associated with the presence of DWT in petrous ICA. We found the phenomenon of DWT in petrous ICA was very prevalent in patients with severe stenosis (≥70%) in intracranial ICA, especially in patients with intracranial ICA occlusion. We also found 38.46% arteries with occluded intracranial ICA had DWT spread from petrous to cervical segment. These arteries showed a certain degree of stenosis not causing by either atherosclerotic plaque or vascular inflammatory disease. We speculate that the long range of DWT causing by intracranial ICA occlusion may also be responsible for some unexplained proximal ICA stenosis, in addition to the decrease in blood flow of the upstream arterial segments. In this study, 3D T1-SPACE (VISTA) was proved to be capable of diagnosing the whole ICA and identifying edema. In conclusion,the diffuse wall thickening of petrous ICA is commonly seen among patients with steno-occlusive disease causing by atherosclerotic plaque in intracranial ICA, especially in occluded intracranial ICA.Acknowledgements
NoneReferences
1.Gibbs, J.M., et al., EVALUATION OF CEREBRAL PERFUSION RESERVE IN PATIENTS WITH CAROTID-ARTERY OCCLUSION. The Lancet, 1984. 323(8372): p. 310-314.
2.Wang, J., V.L. Yarnykh, and C. Yuan, Enhanced image quality in black-blood MRI using the improved motion-sensitized driven-equilibrium (iMSDE) sequence. J Magn Reson Imaging, 2010. 31(5): p. 1256-63.
3.Chen, X., et al., Association between proximal internal carotid artery steno-occlusive disease and diffuse wall thickening in its petrous segment: a magnetic resonance vessel wall imaging study. Neuroradiology, 2017. 59(5): p. 485-490.
4.Chen, X., et al., Proximal internal carotid artery stenosis associates with diffuse wall thickening in petrous arterial segment of moyamoya disease patients: a three-dimensional magnetic resonance vessel wall imaging study. Neuroradiology, 2019. 61(1): p. 29-36.
Figures