2208
Comparison of Myocardial Blood Flow Measurements with Arterial Spin Labeling in Breathhold and Synchronized Breathing Acquisitions1Radiology, Clínica Universidad de Navarra, Pamplona, Spain, 2Universidad Carlos III de Madrid, Madrid, Spain, 3Instituto de Investigación Sanitaria Gregorio Marañón, Madrid, Spain, 4Siemens Healthineers, Madrid, Spain
Synopsis
Arterial spin labeling enables non-invasive quantification of myocardial perfusion. However, there is a need to improve its reproducibility by reducing subtraction errors due to motion and thus, avoiding signal blurring in the acquired low-resolution images. Here, we demonstrate the feasibility of quantifying MBF employing synchronized breathing techniques with FAIR-ASL in healthy subjects. Visually, motion is significantly reduced, MBF values are consistent with those reported in the literature and coefficient of variation for intrasession reproducibility is 13%.
INTRODUCTION
Myocardial arterial spin labeling (ASL) has the potential to quantify myocardial blood flow (MBF) non-invasively. However, its application remains challenging due to the presence of cardiac and respiratory motion. This issue has been typically tackled with the combination of cardiac gating and either breath-holding[1] or free-breathing acquisitions followed by non-rigid registration approaches [2,3]. Less extended in cardiac ASL is the use of respiratory synchronization techniques[4], which have been successfully employed in renal ASL[5]. Synchronized breathing requires subject cooperation to maintain a regular breathing pattern coordinated with the TR of the sequence and a short breathhold during image acquisition. The goal of this work was to assess image quality and intrasession reproducibility of MBF in synchronized breathing (SB) acquisitions with FAIR-ASL.METHOD
Scanning protocol: 4 healthy subjects (age=28±6years, heart rate 53-68bpm) participated in a cardiac MRI study on a 3T Skyra with an 18-channel array coil. The scanning session included: localizers of all chambers of the heart, a short axis cine of the mid-ventricular slice to identify the mid-diastolic phase, followed by a cardiac gated FAIR-ASL sequence with four presaturation pulses, HS adiabatic inversion pulse, single inversion time (TI=1s) and bSSFP readout [FOV: 300x243.8mm2; Matrix: 128x104; GRAPPA-2; Pixel Size: 2.34x2.34x10mm3]. A baseline image was acquired under breathhold for quantification.Breathing strategies: FAIR-ASL acquisitions were acquired during SB. Volunteers were previously trained to recognize the image readout sound. During scanning, they were instructed to inspire and expire after the image readout and then to hold their breath until the end of the next readout. 64 ASL images were acquired with a TR=5s to facilitate a regular breathing pattern. The sequence was repeated to assess intrasession reproducibility. FAIR-ASL images were also acquired under breathhold (BH), including a total of 6 breathholds (~12 seconds duration each), each of them including one pair of label and control images.
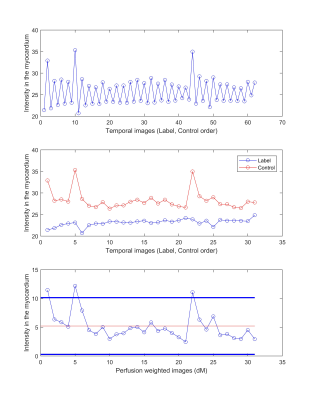
Data processing: Control and label images were pairwise subtracted and averaged. Circular ROIs around the myocardium were manually drawn from the average perfusion-weighted-image in the SB series and from the individual image pairs in the BH acquisitions. Outliers in the $$$\Delta{M}$$$ image series for SB were identified as greater or lower than two standard deviations from the mean. Regional MBF was estimated following equation:
$$$MBF= \frac{C - T}{2 M0 TI e^{-\frac{TI}{T1blood}}} 60000$$$ (ml/g/min)
, where C, T, M0 were the control, tag and baseline image intensities and T1 of blood is 1664ms at 3T. Quality of the images was assessed with the computation of temporal SNR. Coefficient of variation (CV) was calculated to assess intrasession reproducibility.
RESULTS AND DISCUSSION
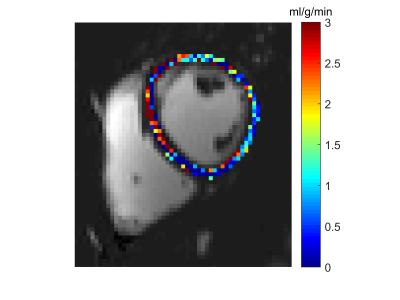
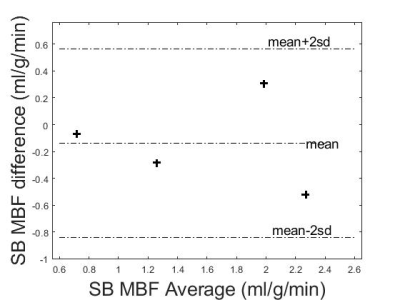
Image quality was visually improved when performing SB acquisitions and minimum motion was observed. Thus, the alternated label-control intensity pattern within the myocardium is clearly visible along the temporal series of images (Fig.1). Figure 2 shows the MBF map of this representative volunteer.Intrasession CV for SB was 13%, considerably lower than the 17.15% achieved in a previously reported free breathing study including image registration [3]. Bland-Altman plot indicates mean ± 2SD MBF differences of -0.14 ± 0.70ml/g/min (Fig.3).
Figure 4 shows that measured MBF values are consistent with those reported in the literature (0.73–2.43 ml/g/min) for asymptomatic human subjects at rest [6]. tSNR varied across volunteers depending on the quality of the synchronized breathing. Although BH acquisitions indicate a superior tSNR, this is not representative as it was computed by averaging only six ASL pairs. For BH acquisitions only, two volunteers present MBF values slightly outside the physiological range (Fig.5).
CONCLUSION
This work demonstrates the feasibility of using SB in cardiac FAIR-ASL acquisitions, thus reducing physiological noise due to motion, reporting an intrasession CV of 11%. A future study will include reproducibility of BH measurements.Acknowledgements
This work has been supported by Asociación de Amigos de la Universidad de Navarra.References
[1] Zun Z, Wong EC, Nayak KS. Assessment of myocardial blood flow (MBF) in humans using arterial spin labeling (ASL): feasibility and noise analysis. Magn Reson Med. 2009;62(4):975-983. doi:10.1002/mrm.22088
[2] Wang DJJ, Bi X, Avants BB, Meng T, Zuehlsdorff S, Detre JA. Estimation of perfusion and arterial transit time in myocardium using free-breathing myocardial arterial spin labeling with navigator-echo. Magn Reson Med. 2010;64(5):1289-1295. doi:10.1002/mrm.22630
[3] Aramendía-Vidaurreta V, García-Osés A, Vidorreta M, Bastarrika G, Fernández-Seara MA. Optimal repetition time for free breathing myocardial arterial spin labeling. NMR Biomed. 2019;(January):e4077. doi:10.1002/nbm.4077
[4] Poncelet BP, Koelling TM, Schmidt CJ, et al. Measurement of human myocardial perfusion by double-gated flow alternating inversion recovery EPI. Magn Reson Med. 1999;41(3):510-519. doi:10.1002/(SICI)1522-2594(199903)41:3<510::AID-MRM13>3.0.CO;2-G
[5] Robson, P. M., Madhuranthakam, A. J., Dai, W., Pedrosa, I., Rofsky, N. M., & Alsop DC. Strategies for reducing respiratory motion artifacts in renal perfusion imaging with arterial spin labeling. Magn Reson Med 2009;61(6)1374–1387.
[6] Chareonthaitawee P, Kaufmann P a, Rimoldi O, et al. Heterogeneity of resting and hyperemic myocardial blood flow in healthy humans. Cardiovasc Res. 2001;50:151-161.
Figures