2200
Differences in Revenues Associated with Magnetic Resonance Angiography versus Computed Tomographic Angiography for Pulmonary Embolism1Radiology, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States, 2Executive MBA, Wisconsin School of Business at the University of Wisconsin-Madison, Madison, WI, United States, 3Accounting and Information Systems, Wisconsin School of Business at the University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Analysis was performed of hospital revenue generated by inpatient, outpatient and emergency department MR and CT angiographic examinations for suspected pulmonary embolism. Negative examinations generated less revenue than examinations positive for pulmonary embolism. Negative MRAs generated slightly more revenue than negative CTAs. Positive MRAs generated more revenue than positive CTAs, however only two MRAs were positive for pulmonary embolism.
Introduction
Contrast-enhanced magnetic resonance angiography (CE-MRA) in the evaluation for pulmonary embolism (PE) prevents patient exposure to ionizing radiation and iodinated contrast agents, and is as effective as computed tomographic angiography (CTA).1,2,3 Several barriers remain to widespread implementation of CE-MRA for PE.4,5 One of these barriers is perceived high cost to patients and hospitals. There is little available data regarding financial differences between CE-MRA and CTA in the United States.Methods
We queried our hospital billing database for all CE-MRA and CTA exams performed to evaluate for pulmonary embolism during the calendar year 2018. Exam type, positivity or negativity for PE, hospital charges and estimated revenue data were obtained. Statistical analyses were performed using Microsoft Excel and RStudio.Results
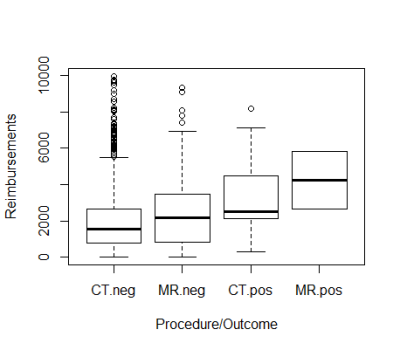
During 2018, a total of 913 exams were found, 3.5% (n=32) of which were positive for pulmonary embolism. Of these exams, 141 were MRA, of which 2.1% (n=3) were positive, and 881 were CTA, of which 3.76% were positive (n=29). Exams included patients of all ages, as well as all visit types (outpatient, inpatient, and emergency department). Outliers were defined as exams associated with hospital revenue of over $10,000. This resulted in exclusion of 50 exams. Statistical analysis was performed of 863 exams: 137 MRA, two of which were positive, and 726 CT, 27 of which were positive. Revenue associated with all exams was nearly $2M.All examinations (CE-MRA and CTA) positive for PE were associated with hospital total revenue of $94,617. Mean and median revenue were $3263 and $2556, respectively, with standard deviation of $2136. All examinations negative for PE were associated with hospital total revenue of $1,861,316; mean and median revenue were $2231 and $1636, respectively, with standard deviation of $1998.
CTAs negative for PE were associated with total reimbursement of $1.5M; mean and median revenue were $2164 and $1527, respectively, with standard deviation of $1981. MRAs negative for PE were associated with total reimbursement of $348,684. Mean and median revenue were $2583 and $2191, respectively, with standard deviation of $2057. CTAs positive for PE were associated with total reimbursement of $86,167. Mean and median revenue were $3191 and $2496, respectively, with a standard deviation of $2154. MRAs positive for PE were associated with total reimbursement of $8450. Mean and median were both $4225, with a standard deviation of $2244.
Conclusions and Discussions
Our data suggest that our institution is reimbursed more when patients do have pulmonary embolism, however this is likely due to length of stay and severity of illness, rather than type of exam performed. Reimbursement for MRAs negative for PE are slightly higher than for CTAs negative for PE. Reimbursement for MRAs positive for PE were higher than for CTAs negative for PE, but this was suboptimal due to being based on only two MRA exams positive for PE.This preliminary analysis is limited. More data is needed. Revenue data was associated only with exam type and result. We were not able to maintain association with any other patient-identifying information, such as age, duration of stay, and baseline patient health. Also, the reimbursement data is only hospital reimbursement. In the US system, physician income is defined as professional fees separate from hospital revenue.
Despite the limitations of this analysis, we suspect the difference in revenue is less than expected by most physicians, and hope this is a small step towards removing institutional barriers for MRA for evaluation for PE.
Acknowledgements
No acknowledgement found.References
1. Schiebler ML, Nagle SK, François CJ, et al. Effectiveness of MR Angiography for the primary diagnosis of acute pulmonary embolism: Clinical outcomes at 3 months and 1 year. J Magn Reson Imaging. 2013 October ; 38(4): 914–925.
2. Benson DG, Schiebler ML, Nagle SK and François CJ. Magnetic resonance imaging for the evaluation of pulmonary embolism. Top Magn Reson Imaging 2017;26:145–151.
3. Benson DG, Schiebler ML, Repplinger MD, François CJ, Grist TM, Reeder SB, et al. Contrast-enhanced pulmonary MRA for the primary diagnosis of pulmonary embolism: current state of the art and future directions. Br J Radiol 2017; 90: 20160901.
4. Nagle SK, Schiebler ML, Repplinger MD et al. Contrast enhanced pulmonary magnetic resonance angiography for pulmonary embolism: Building a successful program. Eur J Radiol. 2016 March ; 85(3): 553–563.
5. Repplinger MD, Nagle SK, Harringa JB, et al. Clinical outcomes after magnetic resonance angiography (MRA) versus computed tomographic angiography (CTA) for pulmonary embolism evaluation. Emergency Radiology (2018) 25:469–477.