2196
Assessment of Apparent Internal Carotid Tandem Occlusion on High-resolution Vessel Wall ImagingComparison With DSA
1Department of Radiology, Tianjin First Central Hospital, Tianjin, China, 2Department of Radiology, First Central Clinical College, Tianjin, China, 3Department of Neurosurgery, Tianjin First Central Hospital, Tianjin, China, 4Department of Radiology, Tianjin Huanhu Hospital, Tianjin, China, 5Department of Neurosurgery, Tianjin Medical University General Hospital, Tianjin, China, 6Department of Neurosurgery, Tianjin TEDA Hospital, Tianjin, China, 7Department of Data statistics, Beijing Hithink Pharmaceutical Technology Service Co.,Ltd, Beijing, China
Synopsis
This study aimed to identify the true ICA tandem occlusions and screen suitability for endovascular recanalization using High-resolution vessel wall imaging (HR-VWI). Patients without blood flow signal in the ICA on MRA who underwent both HR-VWI and DSA was included, and classified into the 4 categories. The suitability for recanalization of occlusion vessels was evaluated. The study showed that about half of patients with an apparent tandem ICA occlusion on DSA, the arteries were, in fact, patent or focal occlusion on VWI. VWI would enable superior identification the true ICA tandem occlusion than DSA.
BACKGROUND AND PURPOSE
Not all tandem occlusions diagnosed on traditional vascular imaging modalities, such as MRA, represent actual completely ICA occlusion. Luminal imaging is sensitive to blood flow, but may misclassify some localized occlusion or near-occlusion as tandem occlusion. This study aimed to explore the utility of High-resolution vessel wall imaging (HR-VWI) in identifying the true ICA tandem occlusions and screening apparent suitability for endovascular recanalization.MATERIALS AND METHODS
Patients with absent signal in ICA on MRA were retrospectively reviewed. All patients underwent HR-VWI on a 3.0 T system (Siemens MAGNETOM Prisma, Germany) with a standard 64-channel head coil. Inversion-Recovery Sampling Refection with Application-optimized Contrasts using different flip angle Evolution (IR-SPACE) sequence was scanned to visualize the intra-lumen status by suppressing blood flow and cerebrospinal fluid signal with the following parameters: TR = 900 ms; TE = 15 ms; 240 slices with slice thickness of 0.55 mm; flip angle = 120°; voxel size = 0.55×0.55×0.55 mm; matrix = 384×336; field of view = 240×210 mm; acquisition time was 7 minutes 43s. Patients exhibited an absence of signal in the ICA on MRA who underwent both HR-VWI and DSA before endovascular treatment were included. Exclusion criteria included: (1) existent signal of the ICA; (2) no DSA images for comparison and reference; (3) insufficient vessel coverage or uninterpretable images due to motion artifact; and (4) nonatherosclerotic or dissection occlusion including Moyamoya disease, vasculitis and trauma. Two neuroradiologists independently reviewed the HR-VWIs to assess whether there were tandem occlusion and categorized all cases into intracranial ICA (IICA) occlusion, extracranial ICA (EICA) occlusion, tandem occlusion, and near-occlusion. DSA images, classified into the same 4 categories, were used as the criterion standard. The length of tandem occlusion also was measured on VWI and DSA respectively. The suitability for recanalization of occlusion vessels was evaluated using the same criteria as those for VWI.RESULTS
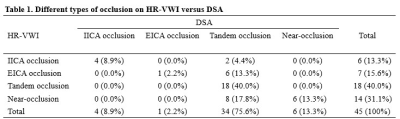
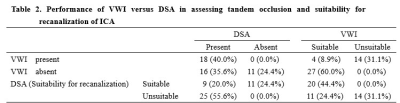
Forty-five patients with absent ICA signal on MRA who had available HR-VWI and DSA images were included in this study. Comparison between VWI and DSA in occlusion category is showed in Figure 1A. Length of occlusion measured on VWI was significantly shorter than that of DSA (P< .0001) (Figure 1B). Eighteen patients (18/45) had tandem ICA occlusion both on VWI and DSA. Among sixteen patients (16/34) with tandem occlusion on DSA, VWI showed IICA occlusion in 2, EICA occlusion in 6, and near-occlusion in 8 (Table 1). Figure 2 depicts an example of the apparent internal carotid tandem occlusion on MRA and pre-operative DSA, whereas VWI showed near-occlusion with completely collapse. The extent of occlusion of 45 patients and their suitablity for recanalization evaluated by DSA and VWI are showed in Figure 3. All of 20 cases (20/45) were considered suitable for recanalization on DSA also contained on VWI. Among 25 patients who were unsuitable for recanalization evaluated on DSA, 11 were found suitable on VWI (Table 2).DISCUSSION
Significant proximal stenosis or occlusion of the extracranial carotid (such as critical atherosclerotic plaque narrowing or dissections) or distal occlusions in the intracranial ICA could give the appearance that the ICA was totally occluded on luminal imaging, the finding was in line with other recent studies.1-3 Previous studies have indicated that even specialized radiologists may not reliably distinguish true cervical occlusion from pseudo-occlusion in patients with ICA nonattenuation at single-phase CT angiography.4 Many studies have advocated the use of DSA to diagnose pseudo occlusion, but in Jonathan et al’s series,5 71% of the patients continued to have a pseudo occlusion on DSA. Thus, the noninvasive VWI, could serve as a more convenient technique for the identification of true ICA tandem occlusion.CONCLUSIONS
VWI would enable superior identification the true ICA tandem occlusion than DSA in patients with absent signal on MRA. Findings on VWI may can be used to screen more suitable candidates for recanalization therapy.Acknowledgements
No Acknowledgement found.References
1. Kim JJ, Dillon WP, Glastonbury CM, et al. Sixty-four-section multidetector CT angiography of carotid arteries: a systematic analysis of image quality and artifacts. AJNR Am J Neuroradiol 2010;31:91-99
2. Duijsens HM, Spaander F, van Dijk LC, et al. Endovascular treatment in patients with acute ischemic stroke and apparent occlusion of the extracranial internal carotid artery on CTA. J Neurointerv Surg 2015;7:709-714 3. Marquering HA, Nederkoorn PJ, Beenen LF, et al. Carotid pseudo-occlusion on CTA in patients with acute ischemic stroke: a concerning observation. Clin Neurol Neurosurg 2013;115:1591-1594
4. Cervical Internal Carotid Occlusion versus Pseudoocclusion at CT Angiography in the Context of Acute Stroke:An Accuracy, Interobserver, and Intraobserver Agreement Study. Radiology 2018
5. Grossberg JA, Haussen DC, Cardoso FB, et al. Cervical Carotid Pseudo-Occlusions and False Dissections:Intracranial Occlusions Masquerading as Extracranial Occlusions. Stroke 2017;48:774-777
Figures
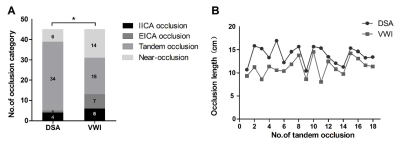
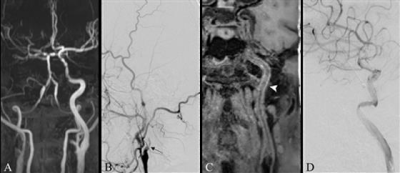
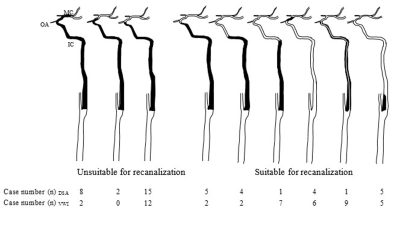
Figure 3. The extent of occlusion of 45 patients and their suitablity for recanalization evaluated by DSA and VWI. The black part represents occlusion or near-occlusion. Subscript DSA or VWI represents evaluated on DSA and VWI.