2192
Dedicated motion-corrected reconstruction for T1-mapping Modified Look-Locker inversion recovery acquisitions1ASL MR, GE Healthcare, Barcelona, Spain, 2GE Healthcare, San Francisco, CA, United States, 3Hospital Clínic de Barcelona, Barcelona, Spain, 4GE Healthcare, Munich, Germany
Synopsis
We present the evaluation results of a new motion correction algorithm, designed specifically to account for the variable image contrast found in T1 mapping MOLLI series.
While standard motion correction improves mapping accuracy with respect to uncorrected series, the registration can occasionally diverge, aggravating the problem. The new dedicated algorithm has been shown to yield improved registration performance and reduced probability of divergence.
INTRODUCTION:
Quantitative relaxation mapping techniques are meeting with increasing success due to their ability to deliver repeatable, objective diagnostic criteria based on non-invasive tissue characterization. Such is the case of myocardial T1 mapping, which has been shown to constitute a reliable indicator of several heart muscle diseases related to changes of myocardial extracellular water (e.g. oedema, fibrosis) as well as fat, iron and amyloid content1,2.T1-mapping techniques typically rely on exponential fitting of a series of sequential relaxation measurements. Precise anatomical alignment between these measurements is key in order to obtain accurate T1 estimates. This is limited by cardiac and respiratory triggering accuracy, as well as by patient bulk motion.
Motion compensation techniques, typically in the form of post-reconstruction image registration, are often applied in order to improve the accuracy of the mapping. In the case of T1-mapping based on MOLLI inversion recovery sequences3, image registration is compromised by the different contrast properties of the frames constituting the relaxation series.
In this study, we present the results of a new MR reconstruction pipeline, including a dedicated image registration method, which accounts for the different intensity properties of the MOLLI series.
METHODS:
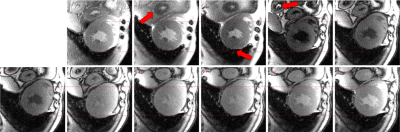
50 patients were included in this study (35 M / 15 F; weight 77±15 Kg; age 62±12), all referrals for a clinically-indicated MRI cardiac scan on a 3.0T GE SIGNA Architect at the Clinical Hospital of Barcelona. The acquisition protocol included, among others, a MOLLI pulse sequence for the purposes of T1 mapping. The acquisition parameters were: 2D bSSFP, Matrix 160x148, Phase FOV 0.8-1.0, 1.4x1.4mm2, ST 8mm, TE 1.4ms, TR 3.0ms, FA 35deg, NEX 1, BW 100kHz, 2x ASSET, 5(3)3, Body 48 1. The raw data of these acquisitions was exported for further analysis.A prototype reconstruction algorithm, implemented using GE Healthcare‘s Orchestra libraries, was used to retrospectively reconstruct all of the exported raw data. The reconstruction consisted of a standard 2D Cartesian pipeline, which mimicked the one implemented in the commercial product. The same pipeline enabled the use of a post-reconstruction frame-by-frame motion correction step. Additionally, a new reconstruction algorithm, including a registration similarity criterion that accounted for the T1 relaxation of tissue, was also applied to all datasets. The algorithm consisted of an iterative approach, alternating polarity estimation, T1 fitting, relaxation series simulation and frame-by-frame registration.
The reconstructed data were automatically analysed to determine the quality of the registration results. The coefficient of determination (R2) of the voxel-wise T1 fitting of the reconstructed image series was used to assess the performance of both registration methods. The results were also reviewed by two board-certified cardiologists with experience in MRI reading and T1 mapping.
RESULTS:
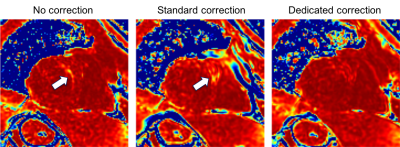
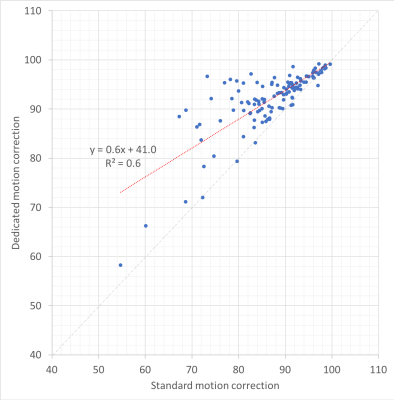
All data were successfully reconstructed with three methods: Uncorrected; With the standard motion correction method; And with the new dedicated method for T1 mapping. Qualitatively correct T1 maps were generated automatically in all cases.The voxel-wise maps of the coefficient of determination showed improvement with either motion correction, in comparison to the uncorrected reconstruction. The improvement could be quantified by considering the number of voxels with R2 > 0.95 in the heart region. In the absence of motion correction, the number of pixels with a high coefficient of determination was 86%±8%. With standard motion correction, this increased to 87%±8%. With the new dedicated method, it further increased to 92%±6%.
With the standard registration method, the T1 mapping performance difference with respect to uncorrected data was 1%±6%; With the new method, this difference increased to 6%±4%. The relative performance of the different methods can be appreciated in Figure 3.
DISCUSSION:
Despite T1 mapping techniques having been repeatedly shown to be a reliable diagnostic tool in cardiac imaging, they remain sensitive to patient motion and triggering inaccuracies, making them vulnerable to arrhythmia episodes. Several instances of misregistration, leading to partially inaccurate T1 maps, were identified in this study. Improving the similarity criterion used by the registration algorithm by accounting for the T1 relaxation of tissue, was found to significantly decrease the incidence of misregistration and subsequent T1 inaccuracies.Quantifying the improvement of T1 mapping with motion correction is not trivial due to the lack of a reliable reference. Using the coefficient of determination of the voxel-wise T1 fit as a surrogate of data alignment quality allowed to confirm the increased robustness of the new, dedicated motion correction method for MOLLI series.
CONCLUSION:
We have demonstrated a new reconstruction pipeline with built-in registration, optimized for MOLLI T1-mapping sequences. The new method has been shown, using clinical data, to improve the robustness to motion of cardiac T1 mapping results.Acknowledgements
No acknowledgement found.References
1. Jellis, C. L. & Kwon, D. H. Myocardial T1 mapping: modalities and clinical applications. Cardiovasc Diagn Ther 4, 126–137 (2014).
2. Radenkovic, D., Weingärtner, S., Ricketts, L., Moon, J. C. & Captur, G. T1 mapping in cardiac MRI. Heart Fail Rev 22, 415–430 (2017).
3. Messroghli, D. R. et al. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 52, 141–146 (2004).
Figures