2170
Association Between Physical Activity and Left Ventricular Diastolic Function and Morphology assessed by MRI in Obesity1Biomedical Engineering and Physics, Amsterdam UMC location AMC, Amsterdam, Netherlands, 2Department of Clinical Epidemiology, Leiden University Medical Center, Leiden, Netherlands, 3Department of Radiology, Leiden University Medical Center, Leiden, Netherlands, 4Department of Cardiology, Leiden University Medical Center, Leiden, Netherlands, 5Department of Radiology, University Medical Center Utrecht, Utrecht, Netherlands, 6Department of Cardiology, Amsterdam UMC location AMC, Amsterdam, Netherlands
Synopsis
Heart failure with preserved ejection fraction is accompanied by diastolic dysfunction. Diastolic dysfunction is associated with metabolic dysregulations, particularly obesity. Physical Activity might reduce this process improving diastolic function and left ventricular (LV) morphology. In this cross-sectional Netherlands Epidemiology of Obesity study, individuals underwent cardiovascular MRI to asses diastolic function and LV Morphology. Physical Activity was determined via the SQUASH questionnaire. Multivariable linear regression was performed adjusting for metabolic covariates. Physical Activity was moderately associated to diastolic function and strongly to LV Morphology. Conclusively, associations of diastolic function and LV morphology with Physical Activity can be determined accurately by MRI.
INTRODUCTION:
Heart failure with preserved ejection fraction (HFpEF) symptomatology is caused by molecular and structural changes in the myocardium, which in turn can be caused by a heterogeneous spectrum of underlying conditions (1). Metabolic dysregulation and a chronic low grade inflamed state are associated with increased diffuse fibrosis and cardiac hypertrophy resulting in a stiffer left ventricle (LV) causing diastolic dysfunction. It has been debated that central (abdominal - visceral) obesity but not general obesity play an important role in the onset and progression of diastolic dysfunction and HFpEF (2). Physical Activity seems to reduce visceral adiposity without change of total body fat (3). Hereby it may have cardio protective effects by reducing metabolic dysregulation promoting diastolic function (4). Cardiac function is often assessed in large scale study’s by echocardiography which is less reliable than MRI (5). In this MRI based study, we therefore hypothesize that Physical Activity was associated with diastolic function and LV morphology, accurately assessed by MRI and may be confounded by effects of metabolic dysregulations particularly central obesity.METHODS:
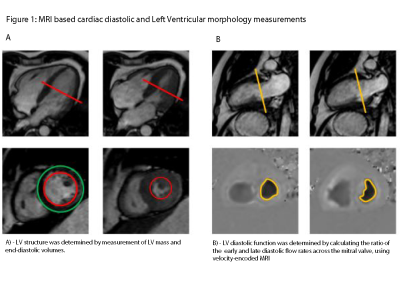
In this cross-sectional analysis of the prospective, population-based Netherlands Epidemiology of Obesity study, 917 middle-aged individuals (53% female, mean age (SD): 56 (6) years) were included after excluding missing data, history of cardiovascular disease and anti-inflammatory medication usage. Participants underwent cardiovascular MRI. For LV structure, the LV was imaged in short-axis orientation using electrocardiographically (ECG)-gated breath-hold balanced steady-state free precession (bSSFP), with imaging parameters: TR/TE 3.4/1.7 ms, FA 35º, slice thickness 10 mm, no slice gap, field of view (FOV) 400x400 mm, matrix size 256x256 (Fig. 1A). To determine diastolic function, an ECG-gated gradient echo sequence with velocity encoding over the mitral valve was used, with imaging parameters: TR/TE 6.5/1 ms, FA 20°, slice thickness 8 mm, FOV 350x350 mm, matrix size 256x256, velocity-encoding gradient 150 cm/s, number of phases 40 (Fig. 1B). Physical Activity was determined via the Short Questionnaire to Assess Health-enhancing physical activity in Metabolic Equivalent of Task (MET) hours per week (h/w). Associations between measures of Physical Activity, divided in quartiles termed as inactive (IN), moderately inactive (MOD-in), moderately active (MOD-ac) and active (AC) and cardiac diastolic markers specified as the ratio between LV transmitral early maximal filling velocity and late filling velocity (E/A ratio), LV mass (LVM), LV mass index (LVMi) and LV end-diastolic volume (LVEDV) where analysed using multivariable linear regression analyses. Covariates were selected on clinical relevance, which where sex and age. Dichotomized Metabolic Syndrome (MS) variables where added specified as central obesity (waist women ≥ 88cm, men ≥ 102cm), hypertriglyceridemia (women/men ≥ 150 mg/dl), low HDL (women < 40 mg/dl, men < 50 mg/dl), hypertension (women/men>130/85 mmHg) and disturbed glucose metabolism (women/men ≥ 100 mg/dl). Dichotomized low-grade systemic inflammation (women/men ≥ 2mg/L) was added as extra element since the MS may linger beyond that predicted by the official MS variables. Total body fat (TBF), measured via bioimpedance in percentages as a continues variable, was added to the model as a measure for general adiposity to adjust the association of central obesity.RESULTS:
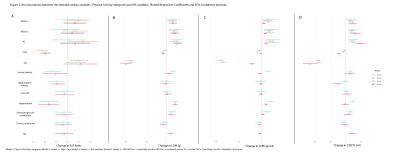
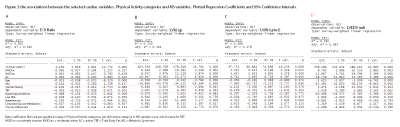
After adjusting for previous mentioned covariates, all Physical Activity categories (IN, MOD-in, MOD-ac and AC) were moderately associated with the E/A ratio after adjusting for previous mentioned covariates (P>0.05, R² = 0.292) – (Fig. 2, Fig. 3). All Physical Activity categories remained strongly associated after adjusting by covariates with LVM, LVmi and LVEDV: MOD-in +6.34g (P=0.002), +2.32g/m2 (P=0.015), +8.69ml (P=0.005), MOD-ac +8.06g (P=0.000), +3.62g/m2 (P=0.000), +12.49ml (P=0.001) and AC +10.92g (P=0.000), +4.71g/m2 (P=0.000), +18.11ml (P=0.000) – (Fig. 2, Fig3). There were no significant statistical interactions between Physical Activity categories and MS variables. Physical Activity Median and interquartile range was 32 MET h/w (15.9 – 53.2). Accordingly, IN was ≤ 15.9 MET h/w, MOD-in was between > 15.9 and ≤ 32 MET/h, MOD-ac was between > 32 and ≤ 53.2 MET/h and AC was > 53.2 MET/hDISCUSSION:
Physical Activity seems to be moderately associated with diastolic function, determined by a positive effect on the E/A ratio. MS variables might have an opposite effect on this association. In particular, hypertension, hypertriglyceridemia and central obesity, but not TBF, may play a role lowering the E/A ratio. Physical Activity seems to be strongly associated with LV morphology, determined by a positive effect on LVM, LVMi and LVEDV after adjusting by all covariates. TBF and central obesity among others have a similar, but smaller effect on this association.CONCLUSION:
MRI based measurements of diastolic function and LV morphology can accurately establish possible associations with Physical Activity.Acknowledgements
No acknowledgement found.References
1. Paulus WJ, Tschope C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263-71.
2. Carbone S, Canada JM, Abbate A. Letter by Carbone et al Regarding Article, "Evidence Supporting the Existence of a Distinct Obese Phenotype of Heart Failure With Preserved Ejection Fraction". Circulation. 2018;137(4):414-5.
3. Belavy DL, Mohlig M, Pfeiffer AF, Felsenberg D, Armbrecht G. Preferential deposition of visceral adipose tissue occurs due to physical inactivity. Int J Obes (Lond). 2014;38(11):1478-80.
4. Borlaug BA, Reddy YN. Getting at the Heart of Central Obesity and the Metabolic Syndrome. Circ Cardiovasc Imaging. 2016;9(6).
5. Grothues F, Smith GC, Moon JC, Bellenger NG, Collins P, Klein HU, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002;90(1):29-34.