2148
Measurement Accuracy of Non-contrast Compressed Sensing Respiratory Motion Resolved Whole Heart MRA in Thoracic Aortic Disease1Medical University of South Carolina, Charleston, SC, United States, 2Siemens Healthcare, Lausanne, Switzerland, 3Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland
Synopsis
Currently, CTA is the only noninvasive method with considerable evidence level for the detection and monitoring of thoracic aortic disease. However, CTA exposes patients to radiation and contrast media. The compressed-sensing whole-heart MRA technique that we evaluated addresses the limitations that prevent conventional MRA techniques to compete with CTA. Our approach eliminates the need for breath-holds or respiratory-navigation, provides a 3D volume of the chest without contrast administration, and allows for accurate anatomical evaluation of the thoracic aorta compared to CTA. Such MRA technique is a potential radiation- and contrast-free alternative for diagnosing and monitoring patients with thoracic aortic disease.
Introduction
Patients with thoracic aortic disease who undergo annual CT angiography (CTA) are subject to repeated radiation and contrast exposure. MRI has weak (level C) indication in such patients. Recently, a novel image reconstruction framework, extradimensional golden-angle radial sparse parallel (XD-GRASP) MRI, was introduced, which integrates the benefits of reduced k-space sampling and sparse reconstruction. Such a technique can be used to reconstruct 3D radial golden-angle coronary artery MRA data acquired during free-breathing at multiple respiratory phases by exploiting the sparsity along the respiratory dimension. The purpose of this proof of concept study was to test and validate this recently developed non-contrast, compressed sensing-based, respiratory motion-resolved whole-heart MRA technique for the anatomical assessment of the thoracic aorta in patients with known thoracic aortic disease in comparison with standard of care CTA.Methods
Twenty-five patients (69±10 years) with known thoracic aortic dilation who underwent clinical CTA were prospectively enrolled for research MRA at 1.5T between July 2017 and November 2018. Whole-heart MRA was performed using a prototype pulse sequence employing a 3D radial trajectory following a spiral phyllotaxis pattern. The following typical imaging parameters were used to image the entire thoracic aorta: TR/TE, 3.1/1.5ms; FOV, (320mm)3; matrix, 1923; isotropic voxel size, (1.66mm)3; flip angle, 115°; and bandwidth, 898Hz/pixel. Raw data were exported offline after the acquisition and processed on a dedicated workstation using a framework implemented in MATLAB. In short: using a respiratory signal extracted directly from the imaging data, the signal-readouts from individual heartbeats of the 3D radial acquisition were binned according to their respiratory phase. The resultant series of undersampled images were then reconstructed using an XD-GRASP algorithm, which exploits sparsity along the respiratory dimension. An end-expiratory phase was used for the subsequent analyses. CTA and MRA images were independently reviewed by two readers. Multi-planar reformat images were used to measure anatomical parameters (area, diameter and circumference) at each level using the double oblique technique. An automated edge detection tool was used with manual correction when needed. Seven anatomical levels of the aorta were measured. A paired Wilcoxon test and Pearson correlation were used to compare CTA and MRA measurements. Bland-Altman plots were used to assess the agreement between MRA and CTA measurements. Interclass correlations (ICC) were used to assess the absolute agreement between readers.Results
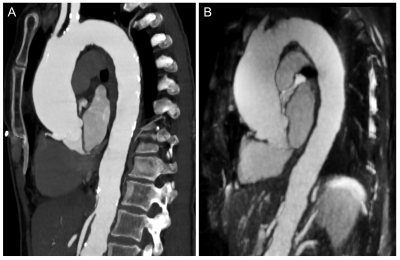
Representative CTA and MRA image examples are shown in Figure 1. No significant differences were observed between CTA and MRA in area (9.7 cm2 [6.8-13.0] vs 9.4 cm2 [6.3-12.7], respectively; p=0.0711), circumference (108.0 mm [90.2-127.0] vs 111.0 mm [92.7-128.0], respectively; p=0.0580), and diameter (35.6 mm [29.8-41.7] vs 35.6 mm [30.0-41.3], respectively; p=0.1085) when performing the comparison on a patient-based level. Similar agreement was found on the level-based analysis. Furthermore, there was excellent correlation between the CTA and MRA measurements (area r=0.93, p<0.0001; circumference r=0.96, p<0.0001; and diameter r=0.92, p<0.0001). Bland-Altman plots also revealed good agreement between the two techniques in the area, circumference and diameter measurements with mean differences of 0.4 cm2 (95% limits of agreement: [-2.4; 3.3]), 2.1 mm [-14.6; 18.7], and -0.3 mm [-6.2; 5.6], respectively. Inter-reader assessment on a patient-based level showed excellent agreement between the readers in both CTA (area ICC=0.9712; circumference ICC=0.9707; diameter ICC=0.8879) and MRA (area ICC=0.9409; circumference ICC=0.9421; diameter ICC=0.9387) measurements. Good to excellent agreement was observed in the level-based assessment with ICCs between 0.6518 and 0.9794.Discussion
While a large variety of MRI techniques have been investigated to detect thoracic aortic disease, most of these conventional approaches have certain limitations preventing them to compete with CTA. Such limitations include the need for breath-holds, the administration of gadolinium-based contrast, the extensively long table time and/or the use of 2D imaging techniques that are less suitable to visualize complex anatomy. The prototype free-breathing whole-heart MRA technique that we evaluated in this work can address all of these limitations as it eliminates the need for breath-holds or respiratory navigation due the respiratory motion-resolved XD-GRASP reconstruction and provides a 3D volume of the chest in a relatively short (~6 minutes) acquisition time without the use of contrast agents. A noteworthy limitation of this technique is the time and computational power needed for image reconstruction. Currently the XD-GRASP reconstruction process is rather time consuming as the iterative algorithm requires several non-uniform Fourier transforms to be performed and the processing time may vary between 10 and 30 minutes based on the workstation configuration available and reconstruction settings used. However, with continued technological improvement, this is not likely to be a long-term obstacle. In conclusion, the free-breathing, whole-heart MRA technique combined with respiratory motion-resolved reconstruction provides comparable anatomical measurements of the thoracic aorta to the reference standard CTA. Thus, this novel and unique MRA technique is a potential radiation- and contrast-free alternative modality for diagnosing and monitoring patients with thoracic aortic disease.Acknowledgements
N/AReferences
1. Piccini D, Feng L, Bonanno G et al. Four-dimensional respiratory motion-resolved whole heart coronary MR angiography. Magn Reson Med 2017;77:1473-1484.21.
2. Feng L, Axel L, Chandarana H, Block KT, Sodickson DK, Otazo R. XD-GRASP: Golden-angle radial MRI with reconstruction of extra motion-state dimensions using compressed sensing. Magn Reson Med 2016;75:775-88.22.
3. Piccini D, Littmann A, Nielles-Vallespin S, Zenge MO. Spiral phyllotaxis: the natural way to construct a 3D radial trajectory in MRI. Magn Reson Med 2011;66:1049-56.