2146
Breath-holding and free-breathing radial-based acquisition strategies for non-contrast MR angiography of the pulmonary veins1Northwestern University, Chicago, IL, United States, 2Northshore University Healthsystem, chicago, IL, United States
Synopsis
CTA and contrast-enhanced MRA (CEMRA) are routinely used to evaluate vascular anatomy prior to pulmonary vein isolation for atrial fibrillation. As potential non-contrast alternatives, we evaluated three radial techniques (breath-hold 2D radial and stack-of-stars (SOS); free-breathing nonselective SOS). 24 patients were studied using CTA as reference standard. Consistently good image quality was obtained with all three radial techniques. There was good-to-excellent agreement with CTA on breath-holding and free-breathing SOS MRA for PV ostial diameters. Our results indicate that radial MRA may provide a useful non-contrast alternative to CTA and CEMRA, with the flexibility of allowing either breath-holding or free-breathing acquisitions.
Introduction
For patients with a history of atrial fibrillation who fail medical therapy, the treatment of choice is pulmonary vein isolation. Pre-procedural evaluation of pulmonary venous (PV) anatomy is typically obtained using CTA or contrast-enhanced MRA (CEMRA)1, 2. For patients who cannot safely tolerate the administration of a contrast agent, free-breathing 3D balanced steady-state free precession (bSSFP) has been described as a potential non-contrast imaging option3. However, vascular detail can be suboptimal due to ghost artifacts and blurring that tend to occur with a Cartesian k-space trajectory or, in some cases, due to irregular breathing patterns that preclude consistent respiratory gating. To minimize these sources of image artifacts, we evaluated the diagnostic performance of both breath-holding and free-breathing non-contrast MRA, using radial k-space trajectories that are known to be less sensitive to flow and motion artifacts than Cartesian4.Methods
24 patients underwent CTA and non-contrast MRA for PV mapping. Three radial MR acquisition strategies were tested: (1) breath-hold 2D radial bSSFP (BH-radial); (2) breath-hold, multiple thin-slab 3D stack-of-stars bSSFP (BH-SOS); and (3) navigator-gated free-breathing 3D stack-of-star bSSFP using a spatially non-selective RF excitation (FB-NS-SOS). Measurements of the maximal and minimal diameters of the PV ostia were obtained from each MRA sequence and compared to CTA. Subjective scoring of the image quality/vessel conspicuity of each MRA sequence was performed using a 5-point scale, ranging from 1: poor quality/non-diagnostic to 5: excellent quality/highly confident diagnosis.Results
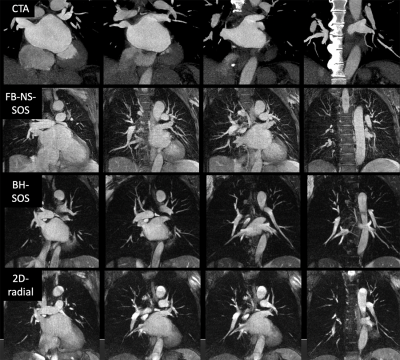
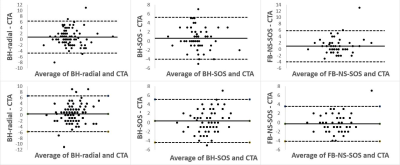
Consistently good image quality was obtained with all three radial MRA techniques (Figure 1), while comparisons with Cartesian 3D in a subset of subjects showed better image quality using radial acquisitions. For PV maximal diameter, there was overall good correlation between BH-radial and CTA (ICC=0.881), excellent correlation between BH-SOS and CTA (ICC=0.915), and good correlation between FB-NS-SOS and CTA (ICC=0.881), all vessels grouped together. For PV minimal diameter, there was overall moderate correlation between BH-radial and CTA (ICC=0.65), good correlation between BH-SOS and CTA (ICC=0.794) and good correlation between FB-NS-SOS and CTA (ICC=0.854), all vessels grouped together. Bland-Altman plots evaluating agreement between CTA and each of the MRA techniques for maximal and minimal PV ostial diameters are shown in Figure 2. BH-SOS showed better overall conspicuity of PV ostia (mean=4.1) compared to BH-radial (mean=3.6) and FB-NS-SOS (mean=4) when all vessels were grouped together (p<0.001). However there was no statistically significant difference of conspicuity between the three non-contrast sequences when each vessel was analyzed separately (mean score raging between 3.3 and 4.8) except for the left inferior pulmonary vein where the score was best on BH-SOS (mean=4.4) compared to BH-radial (mean=3.6) and FB-NS-SOS (mean=4.2) (p<0.05). Off-resonance artifacts were most commonly observed involving the right inferior pulmonary vein ostium and were best suppressed using FB-NS-SOS.Discussion
This study showed that both breath-holding and free-breathing radial MRA were able to depict pulmonary venous anatomy and provide accurate diameter measurements of the ostia. Each radial technique has certain benefits and drawbacks. Compared with 2D radial, stack-of-stars allows for the acquisition of thinner slices with better slice profiles. Unlike the FB-NS-SOS approach which uses a nonselective RF excitation, both 2D radial and thin-slab stack-of-stars MRA allow for substantial flow-related enhancement in the pulmonary veins, thereby improving vessel conspicuity. Moreover, the image quality of breath-hold acquisitions will not be degraded by irregular breathing patterns. On the other hand, FB-NS-SOS has the benefit of requiring less effort by the patient. In addition, the use of a short-duration, nonselective “hard” RF pulse affords a nearly 33% decrease in the sequence repetition time, thereby minimizing signal loss from off-resonance effects with the use of a bSSFP readout.Conclusion
Radial-based MRA techniques provide a promising non-contrast alternative to CTA and CEMRA for PV mapping prior to pulmonary vein isolation, with the flexibility of permitting either breath-holding or free-breathing acquisitions.Acknowledgements
FUNDING SOURCES: NIH grants R01 HL137920 and R01 HL130093
We wish to acknowledge Nondas Leloudas for assisting with scanning and data collection.
References
1. Ghaye B, Szapiro D, Dacher JN, Rodriguez LM, Timmermans C, Devillers D, Dondelinger RF. Percutaneous ablation for atrial fibrillation: The role of cross sectional imaging. RadioGraphics 2003; 23:S19–S33.
2. Wittkampf Fred HM, Vonken EJ, Derksen R, Loh P, Velthuis B, Wever EFD, Boersma LVA, Rensing BJ, Cramer MJ. Pulmonary vein ostium geometry analysis by magnetic resonance angiography. Circulation. 2003;107:21-23.
3. Francois CJ, Tuite D, Deshpande V, Jerecic R, Weale P, Carr JC. Pulmonary vein imaging with unenhanced three-dimensional balanced steady-state free precession MR angiography: initial clinical evaluation. Radiology 2009;250(3):932-939.
4. Glover GH, Pauly JM. Projection reconstruction techniques for reduction of motion effects in MRI. Magn Reson Med 1992;28(2):275-289.
Figures