2135
Plaque Burden of Carotid Atherosclerotic Stenosis Influences Collateral Circulation
Huimin Xu1, Ran Huo1, Ying Liu1, Lizhi Xie2, Ruijing Xin3, Tao Wang1, Huishu Yuan1, and Xihai Zhao4
1Peking University Third Hospital, Beijing, China, 2GE healthcare, Beijing, China, 3Southeastern University, Nanjing, China, 4Center for Biomedical Imaging Research, Beijing, China
1Peking University Third Hospital, Beijing, China, 2GE healthcare, Beijing, China, 3Southeastern University, Nanjing, China, 4Center for Biomedical Imaging Research, Beijing, China
Synopsis
The development of secondary collaterals can be affected by the degree of luminal stenosis, which is not parallel with plaque burden since the positive remodeling effect for elastic arteries. This study aimed to determine the association of carotid plaque burden with status of secondary collaterals in patients with severe carotid stenosis. We found that patients with poor collaterals had significantly larger Max WT than those with good collaterals (7.29 ±1.15 mm vs. 6.59 ± 0.93 mm; P=0.018) when the plaque is larger than 5.45mm.
Background and Purpose
Collateral circulations compensate blood flow for patients with decreased cerebral perfusion. The status of collaterals is significantly associated with clinical outcomes. Secondary collaterals, such as leptomeningeal anastomoses, may be anatomically present, but the enhancement of their capacity likely requires time to develop 1. It is believed that the development of collaterals is heavily dependent on the diminished blood pressure in upstream vessels 2, such as carotid artery luminal narrowing. Since there is positive remodeling effect for elastic arteries, the progression of plaque burden may not be parallel with degree of luminal stenosis 3. However, the relationship between carotid plaque burden and status of secondary collaterals for patients with similar degree of chronic carotid artery stenosis is still unknown. This study aimed to determine the association of carotid plaque burden measured by MR vessel wall imaging with status of secondary collaterals in patients with chronic carotid stenosis.Methods
Study sample: Patients with carotid moderate to severe stenosis (50-99% stenosis) were recruited and underwent CT and MR imaging. The exclusion criteria were as follows: 1) hemorrhagic stroke; 2) cerebral neoplasms; 3) heart failure; 4) renal dysfunction (GFR<60ml/min); 5) iodine contrast agent allergy; 4) contraindications to MR examination. CT perfusion: The whole brain CT perfusion was performed on a 256-row wide-body detector CT scanner with 16 cm z-axis coverage, 0.5 mm slice thickness. It was initiated 8s after contrast agent injection by 10 scans and a 2 s interval, followed by 7 scans and a 4 s interval. The total scan duration was 56s. MR imaging: All patients underwent carotid MR vessel wall imaging on a 3.0T MR scanner with 8-channel carotid coil to acquire the following sequences: 3D time-of-flight, TR/TE 17.6/6.7 ms, flip angle 8°, and slice thickness 2 mm; 2D T1-weighted: TR/TE 850/13.44 ms, slice thickness 2 mm; 2D T2-weighted: TR/TE 2000/96.6 ms, slice thickness 2 mm; and Simultaneous Non-contrast Angiography intraplaque hemorrhage (SNAP) imaging: TR/TE 9.6/4.0 ms, flip angle 12°, and slice thickness 1 mm. The FOV, spatial resolution and longitudinal coverage was respectively 140×140 mm2, 0.55×0.55 mm2, and 32 mm for all imaging sequences. Image review: The collateral circulation score was calculated on multiphase CTA images using a 6-point scale 4. The collaterals were divided into good collaterals (score=4-5) and poor collaterals (score=0-3) status. The plaque components including lipid-rich necrotic core (LRNC), intraplaque hemorrhage (IPH) and calcification (CA) were identified and the Max WT and luminal stenosis were measured for the index artery with most severe stenosis bilaterally. Statistics: Carotid plaque features were compared between patients with good and poor collaterals using Mann-Whitney U test or Chi-square. Univariate and multivariate logistic regressions were used to determine the correlation between plaque features and poor secondary collaterals.Results
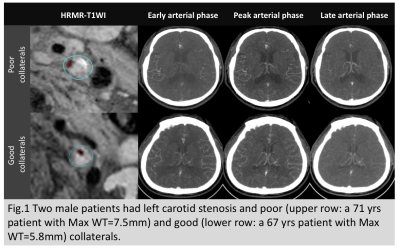
Of 140 included subjects (mean age, 65.5±7.8 years; 122 males), 121 (86.4%), 137 (97.9%), and 97 (69.3%) had carotid CA, LRNC, and IPH, respectively. No significant differences were found in prevalence of plaque components and Max WT between patients with poor and good collaterals in all patients (all p>0.05,Table 1). Patients were divided into 2 groups according to the median of Max WT (5.45 mm): large plaque group (Max WT >5.45) and small plaque group (Max WT ≤5.45). In large plaque group, patients with poor collaterals had significantly larger Max WT than those with good collaterals (7.29 ±1.15 mm vs. 6.59 ± 0.93 mm; P=0.018, Fig. 1). Max WT was significantly correlated with poor collaterals after (odds ratio, 2.07; 95% CI, 1.14 to 3.76, P=0.018) adjusted for clinical risk factors and carotid stenosis. No significant correlations were found between other plaque features and poor collateral status (all P>0.05, Table 1). In small plaque group, no significant correlations were found between plaque features and poor collateral status (all P>0.05, Table 1).Discussions
This study examined the association of carotid plaque features with status of secondary collaterals in patients with chronic carotid stenosis. We found that there were no significant correlations between plaque features and collateral status when the plaque burden is relatively small (Max WT ≤5.45). In contrast, when the plaque burden is large (Max WT >5.45), we found that patients with larger Max WT had poorer collaterals. While the other plaque features will not influence the secondary collaterals.Conclusions
When the plaque burden reaches a certain level, carotid artery Max MT is independently associated with secondary collateral status, suggesting that the continually increase of plaque will worsen the secondary collateral status.Acknowledgements
No acknowledgementsReferences
[1]. Stroke. 2003;34:2279-84.
[2]. Neurology. 1957;7:447-58
[3]. 2011;42:347-53.
[4]. Radiology. 2015;275:510-20.