2131
Hypertension is Associated with the Diffuseness of Intracranial Atherosclerotic Disease: a Cross-sectional MR Vessel Wall Imaging Study1Cedars-Sinai Medical Center, Los Angeles, CA, United States, 2Hospital of the University of Pennsylvania, Philadelphia, PA, United States, 3Beijing Xuanwu Hospital, Beijing, China, 4Beijing Chaoyang Hospital, Beijing, China, 5University of California, Los Angeles, Los Angeles, CA, United States
Synopsis
Hypertension is associated with intracranial atherosclerosis and cerebrovascular events. However, the correlation between hypertension and atherosclerosis disease burden (the number, distribution
Introduction
Hypertension is a major risk factor for intracranial atherosclerosis disease (ICAD)1. However, the correlation between hypertension and ICAD burden (such as plaque number, distribution, and incidence of vulnerable plaque features) remains unclear. MR vessel wall imaging (MR-VWI) has emerged as a non-invasive modality that can directly visualize the intracranial vessel wall and characterize ICAD2. Our study aimed to use MR-VWI to investigate the hypertension-ICAD relationship in a symptomatic ICAD patient cohort.Methods
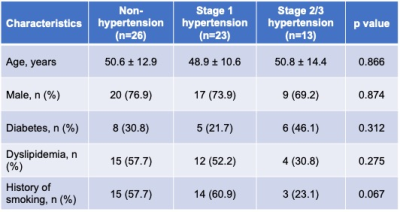
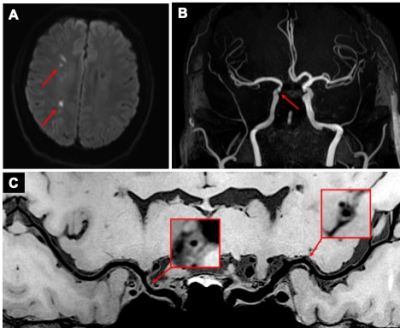
We retrospectively enrolled 62 ischemic stroke patients (46 M, age 50.0 years±12.2) from our institutional MR-VWI database. The inclusion criteria were as follows: (1) acute or subacute ischemic stroke in the territory of the anterior circulation caused by ICAD; (2) at least one >30% intracranial stenosis within the vascular territory of the stroke, confirmed by MRA or CTA; (3) at least one atherosclerotic risk factor, such as hypertension, diabetes mellitus, dyslipidemia, and history of smoking. All MR images were obtained on a 3T system (MAGNETOM Prisma or Verio, Siemens, Erlangen, Germany) equipped with a 64-channel head-neck coil (Prisma) or 32-channel head coil (Verio). The protocol included DWI, 3D TOF-MRA, pre-contrast MR-VWI. MR-VWI was performed using a recently developed 3D whole-brain VWI sequence3 with the following parameters: TR/TE = 900/15 ms; field of view = 170×210 mm2/170×170 mm2; voxel size = 0.55/0.53 mm isotropic; scan time = 8 minutes. All plaques identified in the large intracranial arteries of the anterior circulation were analyzed. The high signal intensity on T1WI (HST1) feature was defined if a plaque showed >1.5 times signal intensity of normal vessel wall. A proximal plaque was defined as the one located at the intracranial internal carotid artery (ICA), A1 segment of the anterior cerebral artery (A1-ACA) and M1 segment of the middle cerebral artery (M1-MCA). A distal plaque was defined as the one located at A2-ACA and M2/M3-MCA. Demographic data and clinical diagnoses were collected. The patients were divided into three groups (non-hypertension, stage 1 hypertension and stage 2/3 hypertension) based on 2003 WHO hypertension criteria4. Pearson’s Chi-squared test and one-way ANOVA test were used to evaluate the differences in age, sex and risk factors among the three groups. One-way ANOVA was used to assess the differences in the total number of plaques, number of proximal plaques, number of distal plaques, and number of HST1 lesions among the three groups. A multivariate linear regression model was used to assess the associations between total number of intracranial atherosclerotic plaques, number of proximal plaques and number of plaques with HST1 in the anterior circulation. Significance was set to p<0.05.Results
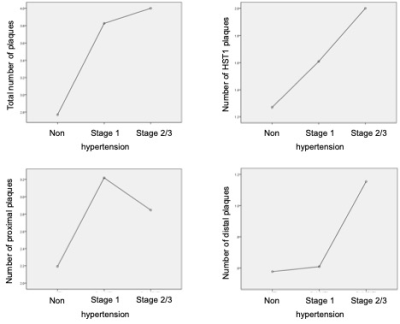
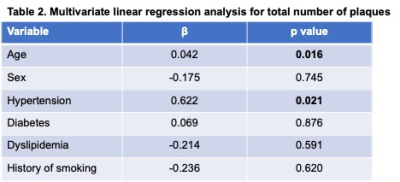
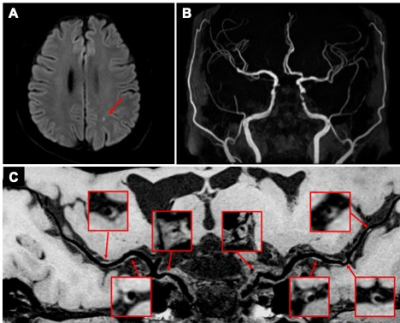
In the cohort, 26 patients were categorized into the non-hypertension group (blood pressure <140/90 mmHg), 23 were categorized into the stage 1 hypertension group (systolic 140-159 mmHg and/or diastolic 90-99 mmHg), and 13 were categorized in the stage 2/3 hypertension group (systolic ≥160mmHg and/or diastolic ≥100mmHg) (Table 1). The average number of plaques was 2.77±1.03, 3.83±1.48 and 4.00±2.31 in these groups respectively. The average numbers of plaques with HST1 were 1.27±0.72, 1.61±0.34 and 2.00±2.31 and the numbers of proximal plaques were 2.19±0.80, 3.22±1.41 and 2.85±1.57, respectively. Significant differences emerged among the three groups in the total number of plaques (p=0.023) and total number of proximal plaques (p=0.018), whereas no significant difference was seen in the total number of HST1 plaques (p=0.307) or distal plaques (p=0.097) (Figure 1). Multivariate regression analysis showed that age (β=0.04, p=0.016) and a diagnosis of hypertension (β=0.62, p=0.021) were significantly associated with the total number of intracranial plaques in the anterior circulation after accounting for age, sex, smoking history and diagnoses of diabetes and dyslipidemia (Table 2). Representative cases of the non-hypertension group (Figure 2) and hypertension group (Figure 3) are shown.Discussion
Our results show that hypertension is significantly associated with ICAD lesions. The significantly higher number of proximal plaques in hypertension groups suggests that high blood pressure tends to affect proximal arterial segments. Grade of hypertension is significantly associated with the total number of plaques at the anterior circulation. These findings are in line with the pathology that hypertensive arteries are thickened, and there may be increased smooth muscle cell mass and/or cell number and increased deposition of connective tissue. In studies of carotid arteries, similar results show strong associations between hypertension and atherosclerosis5.Conclusion
MR-VWI reveals a significant association between hypertension and the total number of plaques at the anterior circulation in symptomatic ICAD patients. This suggests that hypertension is an important mechanistic factor for diffuse intracranial atherosclerosis. Further studies with the inclusion of asymptomatic ICAD patients are warranted.Acknowledgements
No acknowledgement found.References
1. Alexander RW. Theodore cooper memorial lecture. Hypertension and the pathogenesis of atherosclerosis. Oxidative stress and the mediation of arterial inflammatory response: A new perspective. Hypertension. 1995;25:155-161
2. Dieleman N, Yang W, Abrigo JM, Chu WC, van der Kolk AG, Siero JC, et al. Magnetic resonance imaging of plaque morphology, burden, and distribution in patients with symptomatic middle cerebral artery stenosis. Stroke. 2016;47:1797-1802
3. Fan Z, Yang Q, Deng Z, Li Y, Bi X, Song S, et al. Whole-brain intracranial vessel wall imaging at 3 tesla using cerebrospinal fluid-attenuated t1-weighted 3d turbo spin echo. Magn Reson Med. 2017;77:1142-1150
4. Afridi I, Canny J, Yao CH, Christensen B, Cooper RS, Kadiri S, et al. 2003 world health organization (who)/international society of hypertension (ish) statement on management of hypertension. Journal of Hypertension. 2003;21:1983-1992
5. Liu AY, Yu ZQ, Wang N, Wang WH. Carotid atherosclerosis is associated with hypertension in a hospital-based retrospective cohort. International Journal of Clinical and Experimental Medicine. 2015;8:21932-21938
Figures