2124
Comparison of plaque characteristics between patients with small and large subcortical infarction using high resolution MR vessel wall imaging
Na Zhang1, Tingting Zhu2, Lijie Ren3, Lei Zhang1, Zhangyan Fan3, Liwen Wan1, Hairong Zheng1, and Xin Liu1
1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, 2Department of Radiology, Tongji Hospital, Wuhan, China, 3Department of Neurology, Shenzhen Second People's Hospital, Shenzhen, China
1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, 2Department of Radiology, Tongji Hospital, Wuhan, China, 3Department of Neurology, Shenzhen Second People's Hospital, Shenzhen, China
Synopsis
It is generally believed small subcortical infarction (SSI) (also termed lacunar stroke) is caused by intrinsic diseases of penetrating arteries. Recent studies have shown the incidence of atherosclerosis in large arteries which is an important pathogenesis of large subcortical infarction (LSI) is also high in patients with SSI. This indicates the underlying mechanisms of SSI in patients with large artery atherosclerosis may be the same with LSI and inferred from plaque characteristics. However, the plaque characteristics ultimately leading to SSI or LSI remain unclear. This study is to explore the differences of plaque characteristics between patients with SSI and LSI.
Introduction
Small subcortical infarction (SSI) (also termed lacunar stroke) accounts for about 25% of ischemic strokes and is commonly occurred on middle cerebral artery (MCA) territory.1 It is generally believed that SSI is caused by intrinsic diseases of penetrating arteries themselves.2 Several recent studies have shown that the incidence of atherosclerosis in large arteries which is an important pathogenesis of large subcortical infarction (LSI) is also high in patients with SSI.3,4 This indicates the underlying mechanisms of SSI in patients with large artery atherosclerosis may be the same with that causing LSI and inferred from plaque characteristics. However, the plaque characteristics ultimately leading to SSI or LSI remain unclear. High-resolution magnetic resonance vessel wall imaging (HR-MRVWI) has demonstrated the potential to depict large arterial vessel wall lesions and characterize plaques and proven to be reproducible.5-8 The aim of this study is to explore the differences of plaque characteristics on MCA between patients with SSI and LSI using HR-MRVWI.Materials and Methods
The study was approved by the local institutional review board. Informed consent was obtained from all patients. From 2017 to 2019, Seventy-one patients (mean age, 47.49±11.5 years; 55 men) with recent ischemic stroke were prospectively enrolled with the following inclusion criteria: (1) first time acute ischemic stroke located subcortical within unilateral MCA territory identified by T2W-FLAIR; (2) lack of coexistent ipsilateral internal carotid artery with significant stenosis (≥50%) as confirmed by MRA, CTA, or DSA; (3) no evidence of other stroke mechanisms (coagulopathy, a potential cardioembolic source of disease, Moyamoya disease, dissection, etc). All patients underwent routine brain MRI (T1w- and T2w-FLAIR) and HR-MRVWI examinations within four weeks of symptom onset on a 3T MR system (Siemens Trio) with a custom designed 32-channel head-neck coil. Patients were divided into two groups by two experienced neurologists in consensus according to the size of the lesion on T2-FLAIR images: (1) Patients with maximal axial lesion diameter of ≤ 20 mm (SSI group).9 (2) Patients with larger lesions which were not categorized as SSI, including large deep perforator infarcts, border zone infarcts and superficial perforator infarcts (LSI group).10 A cross-sectional slice of the most stenotic location of MCA on the ipsilateral side of cerebral infarction and a cross-sectional slice of the contralateral normal vessel were reconstructed for assessing plaque distribution (superior, inferior, dorsal, or ventral side of the vessel),11 plaque burden, remodeling pattern (positive, intermediate or negative),12 and stenosis degree. In the case of two or more quadrants are involved, the location and number of quadrants were recorded. The patient demographics and the above plaque characteristics were statistically compared between the two groups.Results
Of the 71 patients, 43 (60.6%) were determined as SSI and 28 (39.4%) were LSI. Patient demographics are presented in Table 1. No significant difference were found. No wall thickening was found on five patients with SSI (11.6%). The comparison of the number of quadrants with plaque formation and location of plaque distribution between groups were listed in Table 2 and 3 respectively. The plaques of 13 patients with SSI involved only one quadrant, and the proportion was significantly higher than that of LSI (34.2% versus 7.1%, P=0.006). In addition, the 13 plaques were more frequently located in the superior (46.2%) and dorsal sides (38.5%). The occurrence of plaque involving two or more quadrants was roughly the same between the groups, and plaques involving two quadrants was the most in both groups, 17 and 19 plaques in SSI and LSI, respectively. The location of plaque distribution in four quadrants between the two groups was similar. The ventral side was a relatively common involved quadrant, while the dorsal side was a relatively less involved quadrant. There was no significant difference of plaque burden between groups (0.75±0.12 versus 0.79±0.10, P=0.162). The remodeling pattern and stenosis degree between groups were shown in Figure 1. Most of the plaques in both groups exhibited positive remodeling (52.6% in SSI and 53.6% in LSI). There was no significant difference of the percentage of remodeling patterns, but a significant higher incidence of low-grade stenosis (<50% stenosis) was observed in SSI than LSI (68.4% versus 42.9%, P = 0.037). More patients showed moderate to severe stenosis (≥50% stenosis) in LSI group (Figure 2).Discussion and Conclusion
The results of this study suggested that SSI maybe related to MCA atherosclerosis and the plaque distribution may play an important role. High plaque burden (>70%) and percentage of positive remodeling (>50%) were found in both groups. This is because the patients recruited are symptomatic and hence the plaques analyzed may be vulnerable. These similar plaque features between the groups also suggested that SSI maybe not a mild form of LSI in large arterial atherosclerosis. The lower stenosis degree of SSI may not affect the whole vascular territory as LSI with relatively higher stenosis, but the specific location of the plaque may obstruct the blood flow of perforator artery and will lead to a smaller infarction. In conclusion, both SSI and LSI maybe associated with major intracranial arterial atherosclerosis. But patients with SSI show a relatively fewer number of quadrants with plaque formation and slighter degree of stenosis.Acknowledgements
This work was supported in part by National Natural Science Foundation of China (81830056 and 81801691), Natural Science Foundation of Guangdong Province (2018A030313204), Shenzhen Basic Research Program (JCYJ20180302145700745 and JCYJ20170413161350892).References
1. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010; 9(7):689-701. 2. Caplan LR. Intracranial branch atheromatous disease: a neglected, understudied, and underused concept. Neurology. 1989; 39(9):1246-50. 3. Xu WH, Li ML, Niu JW, et al. Intracranial artery atherosclerosis and lumen dilation in cerebral small-vessel diseases: a high-resolution MRI Study. CNS Neurosci Ther. 2014; 20(4):364-7. 4. Zou XD, Chung YC, Zhang L, et al. Middle Cerebral Artery Atherosclerotic Plaques in Recent Small Subcortical Infarction: A Three-Dimensional High-resolution MR Study. Biomed Res Int. 2015; 2015:540217. 5. Fan Z, Yang Q, Deng Z, et al. Whole-brain intracranial vessel wall imaging at 3 Tesla using cerebrospinal fluid-attenuated T1-weighted 3D turbo spin echo. Magn Reson Med 2017; 77(3):1142-1150. 6. Zhang L, Zhang N, Wu J, et al. High resolution simultaneous imaging of intracranial and extracranial arterial wall with improved cerebrospinal fluid suppression. Magn Reson Imaging. 2017; 44:65-71 7. Zhang N, Zhang F, Deng Z, et al. 3D whole-brain vessel wall cardiovascular magnetic resonance imaging: a study on the reliability in the quantification of intracranial vessel dimensions. J Cardiovasc Magn Reson. 2018; 20(1):39. 8. Wan L, Zhang N, Zhang L, et al. Reproducibility of simultaneous imaging of intracranial and extracranial arterial vessel walls using an improved T1-weighted DANTE-SPACE sequence on a 3 T MR system. Magn Reson Imaging. 2019; 62:152-158. 9. Wardlaw JM. What causes lacunar stroke? J Neurol Neurosurg Psychiatry. 2005; 76(5):617-9. 10. Bogousslavsky J, Regli F. Centrum ovale infarcts: subcortical infarction in the superficial territory of the middle cerebral artery. Neurology. 1992; 42(10):1992-8. 11. Xu WH, Li ML, Gao S, et al. Plaque distribution of stenotic middle cerebral artery and its clinical relevance. Stroke. 2011; 42(10):2957-9. 12. Qiao Y, Anwar Z, Intrapiromkul J, et al. Patterns and Implications of Intracranial Arterial Remodeling in Stroke Patients. Stroke. 2016; 47(2):434-40.Figures
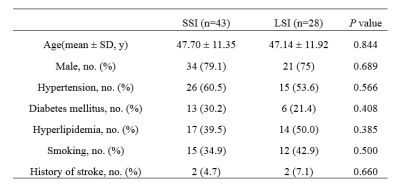
Table
1 Clinical demographics of the patients with SSI and LSI.
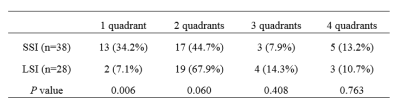
Table 2 Comparison of the number of quadrants with plaque
formation between SSI and LSI groups.
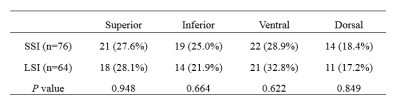
Table
3 Comparison of the location of plaque distribution between SSI and LSI groups.
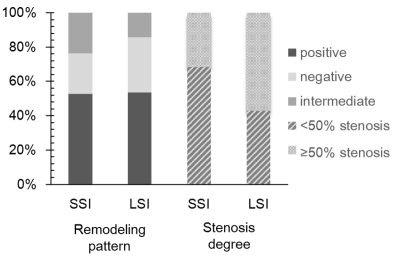
Figure
1 Percentages of remodeling patterns (positive, intermediate, and negative) and
of stenosis degrees (< 50% and ≥ 50% stenosis) between two groups.
Figure
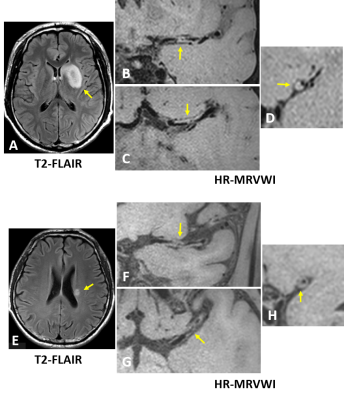
2 Representative MRI images of two patients with LSI (A-D) and SSI (E-H),
respectively. T2-FLAIR images (A and E) show the subcortical infarction in left
middle cerebral artery (MCA) territory (arrows). A plaque (arrows) was detected
at the ipsilateral MCA on HR-MRVWI images (B, C, F, and G) for each patient.
The cross-sectional images (D and H) show the plaques involved three quadrants,
respectively. But the plaque of the patient with LSI (D) caused more stenosis
than the patient with SSI (H).