2120
Higher plaque burden of middle cerebral artery is associated with recurrent ischemic stroke: a quantitative study by high-resolution MRI1Department of Radiology, Sichuan Provincial People's Hospital, Chengdu, China, 2Department of Magnetic Resonance, The first Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 34. Interventional department, The first Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 4Yale School of Medicine and Yale University, New Haven, CT, United States, 5MR Collaboration, Siemens Healthcare Ltd., Beijing, China, 63. Department of Radiology and Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States
Synopsis
Middle cerebral artery plaque burden on high-resolution MR was significantly higher in recurrent stroke group than in the first-onset acute stroke and chronic stroke groups (p=0.002). Patients with acute stroke had higher enhancement ratio than patients with chronic stroke (p=0.014). After adjustment of clinical demographic factors, plaque burden was the only independent imaging feature associated with recurrent stroke (odds ratio=2.26, per 10% increase, 95% CI, 1.03-4.96, p=0.042). In conclusion, higher plaque burden of MCA on MR is independently associated with recurrent ischemic stroke. MR vessel wall imaging may provide unique information for risk stratification of stroke patients.
Introduction
Despite intensive medical management, ICAS is associated with a considerable risk of ischemic event recurrence (as high as 10-24% annually) and fatal outcomes [1,2]. Determination of factors associated with stroke recurrence can help optimize clinical management to prevent future strokes. High-resolution black- blood magnetic resonance (MR) vessel wall imaging has been reported as a reproducible and effective technique to identify and characterize atherosclerotic lesions including plaque morphology, composition and enhancement [3,4]. However, the association between plaque features and stroke recurrence is poorly understood. This study aims to investigate the association between the characteristics of atherosclerotic plaques of middle cerebral artery (MCA) and recurrent ischemic stroke using magnetic resonance (MR) vessel wall imaging.Methods
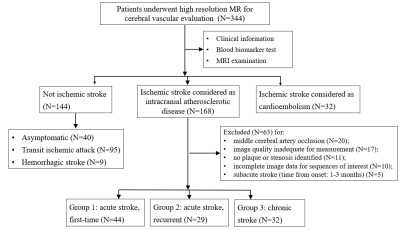
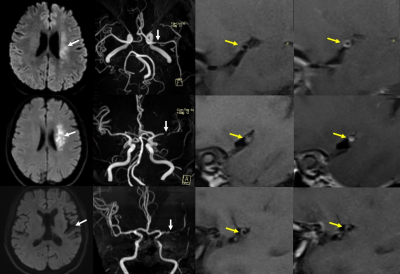
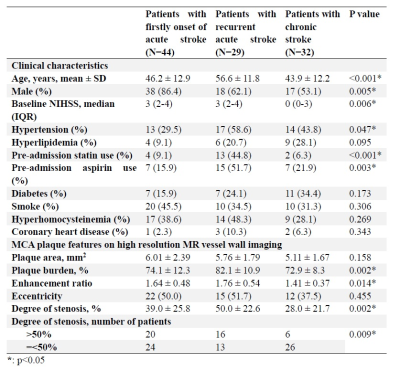
One hundred and five patients with ischemic strokes attributed to MCA plaques underwent high-resolution black-blood MR vessel wall imaging on 3.0 T scanners. Pre-and post-contrast T1-weighted fast-spin-echo sequences were employed (TR/TE=430/10 ms; echo train length (ETL)=9; number of excitations (NEX)=6, slice thickness=2mm, in-plane resolution=0.55 mm x 0.53 mm). The patients were divided into group 1, with the first episode of acute stroke (imaging within one month of stroke, N=44); group 2, with recurrent acute stroke (N=29); and group 3, with chronic stroke (imaging after three months of stroke, N=32). Plaque characteristics including plaque area, plaque burden, contrast enhancement ratio, eccentricity and degree of stenosis were measured and compared across three groups. Association between plaque characteristics and recurrent strokes were investigated by univariate and multivariate analysis.Results
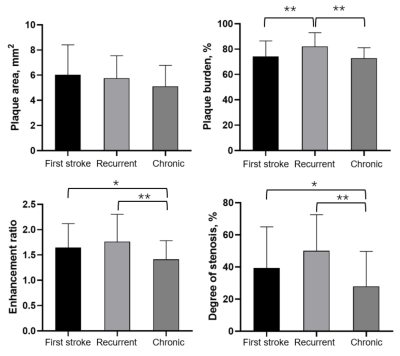
Plaque burden was significantly greater in recurrent stroke group than the other two groups (group 2, 82.1% ± 10.9%, vs. group 1, 74.1% ± 12.3% and group 3, 72.9% ± 8.3%, p=0.002). Patients with acute stroke had higher enhancement ratio than patients with chronic stroke (group 1, 1.64 ± 0.48 and group 2, 1.76 ± 0.54, vs. group 3, 1.41 ± 0.37, p=0.014). Comparing to first-onset acute stroke patients, recurrent stroke patients were older, more likely with female gender and hypertension, and had higher plaque burden. After adjustment of clinical demographic factors, plaque burden was the only independent imaging feature associated with recurrent stroke (odds ratio=2.26, per 10% increase, 95% CI, 1.03-4.96, p=0.042).Discussion
Recurrent stroke, which might indicate the failure of medical therapy, may lead to greater disability, increased risk of dementia, and mortality risk [5]. This study offers more direct evidence of plaque burden being an independent factor associated with recurrent strokes. Such biomarker can be potentially used to predict recurrence risk for stroke patients, and thereby enable tailoring of treatment strategies and initiation of more aggressive therapies.Compared to the absolute value of plaque area, plaque burden uniquely accounts for both the magnitude of lumen narrowing and the arterial remodeling patterns. It thus provides greater insights as to whether the accommodation by remodeling is capable of preserving the lumen. Using high-resolution MRI to monitor the change of plaque burden overtime in future studies may have great clinical implications, because after the first stroke event, plaque can either respond to medical therapy and stabilize, or progress and lead to a recurrent event.
Atherosclerotic plaque enhancement detected by using gadolinium contrast agent has been proposed as a biomarker related to strokes [6]. In this study, however,no significant difference in enhancement ratio was detected between group 1 and group 2. This indicates that the enhancement seen during the acute stroke phase might imply a less specific pathophysiological process with limited positive predictive value for recurrence.On the other hand, our study suggests that the plaque enhancement ratio might decrease over time as the plaque becomes stabilized, indicating the potential negative predictive value of plaque enhancement.
The degree of stenosis of MCA remains a widely used parameter for clinical management [7]. Multivariate analysis of our study showed that the association between plaque burden and stroke recurrence was independent of the degree of stenosis, indicating the importance of plaque evaluation uniquely provided by vessel wall imaging.
Conclusion
In conclusion, our study found higher plaque burden to be independently associated with recurrent ischemic stroke. MR vessel wall imaging may provide unique information for risk stratification of stroke patients, and these imaging markers should be tested in future clinical trials.Acknowledgements
/References
[1] Wong KS, Li H. Long-term mortality and recurrent stroke risk among Chinese stroke patients with predominant intracranial atherosclerosis. Stroke. 2003;34:2361-2366 6.
[2] Mazighi M, Tanasescu R, Ducrocq X, Vicaut E, Bracard S, Houdart E, et al. Prospective study of symptomatic atherothrombotic intracranial stenoses: The gesica study. Neurology. 2006;66:1187-1191.
[3] Zhang X, Zhu C, Peng W, Tian B, Chen L, Teng Z, et al. Scan-rescan reproducibility of high resolution magnetic resonance imaging of atherosclerotic plaque in the middle cerebral artery. PLoS One. 2015;10:e0134913.
[4] Mandell DM, Mossa-Basha M, Qiao Y, Hess CP, Hui F, Matouk C, et al. Intracranial vessel wall mri: Principles and expert consensus recommendations of the american society of neuroradiology. AJNR Am J Neuroradiol. 2017;38:218-229.
[5] Hardie K, Hankey GJ, Jamrozik K, Broadhurst RJ, Anderson C. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the perth community stroke study. Stroke. 2004;35:731-735.
[6] Huang J, Jiao S, Zhao X, Zhang J, Zhang C, Chen M, et al. Characteristics of patients with enhancing intracranial atherosclerosis and association between plaque enhancement and recent cerebrovascular ischemic events: A high-resolution magnetic resonance imaging study. Acta Radiol. 2019;60:1301-1307.
[7] Warfarin-Aspirin Symptomatic Intracranial Disease Trial I. Design, progress and challenges of a double-blind trial of warfarin versus aspirin for symptomatic intracranial arterial stenosis. Neuroepidemiology. 2003;22:106-117.
Figures