2112
Stent effects in 2D and 4DFlow investigation: should we stop using stainless-steel stents?1GE Healthcare, Munich, Germany, 2GE Healthcare, London, United Kingdom, 3GE Healthcare, Sunnyvale, CA, United States, 4German Heart Center Munich, Munich, Germany, 5TUM, Munich, Germany
Synopsis
Flow measurements using Phase Contrast MRI in the present of stents is of clinical relevance, especially in vessels with no alternative to measure elsewhere. Here, we evaluate 4 different stent types in a pulsatile flow phantom using both 2D and 4DFlow including different acquisition schemes for 4DFlow, e.g. 1 slab whole-volume, 1slab with reduced number of slices and multislab whole-volume. The stent made of platinum-iridium was the only stent under evaluation that allowed in-stent accurate net flow measurements for both 2D and 4DFlow (1 slab with reduced number of slices and multislab whole-volume).
Introduction
There are very few works investigating effects of stents in the net flow calculation using Phase Contrast (PC) MRI1. Measuring net flow within or close to the stent is of clinical relevance since in some vessels there is no possibility to measure elsewhere (e.g. left or right pulmonary artery, or main pulmonary artery). In this work, we aim to evaluate four different stents including one made of platinum-iridium which it is expected to create less susceptibility artifacts in all PC MR images, in a flow phantom setup using 2D and 4D Flow.Methods
Stents: Four stents were analyzed, namely, type A: Visipro ev made of stainless steel, type B: Intrastent – Max LD Stent ev3 made of stainless steel, type C: Melody Platinum-Iridium, type D: Cook 316L stainless steel.Acquisition: We used a closed-circuit pulsatile flow phantom2; comprised of an industrial membrane flow pump, an agar box containing two silicone tubes in a u-shaped connection and a Coriolis flow meter (PROMASS 83F08, Endress+Häuser), to measure a ground-truth net flow value with a precision of ±0.5ml/s. The gating signal was obtained by pulsioxymetry in the inflow tube. Flow phantom scans were performed on a GE 3.0T MR750w (Waukesha, WI).
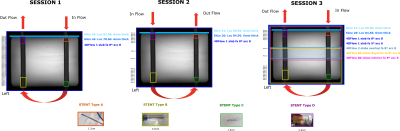
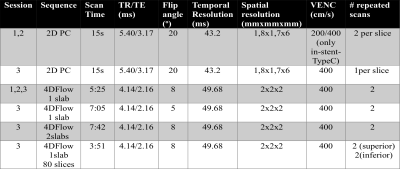
Three different sessions were scanned using the same setup. In session 1, partially overlapped 2D slices (45) were scanned covering the whole phantom volume and 1 slab 4DFlow with flip angle 8 º repeated twice were scanned to evaluate reproducibility. Scans were repeated before and after placing the stents. Fluid flew left to right during session 1. In session 2, the same phantom with the stents was scanned with inverted flow direction (right to left) in order to evaluate possible effects of downstream flow measurements dependent on the stent position. In order to rule out any influence of lower SNR/VNR in 4DFlow3 with respect to 2D Flow, in session 3, 2D PC was done with VENC 400 cm/s and other acquisition schemes for 4DFlow were added to increase SNR/VNR (reduced flip angle and acceleration and 2 slabs) and to separate the acquisition of stents in the inferior and superior side of the phantom (2 slabs and reduced coverage in z-direction so that each slab acquisition was covering 2 stents at a time (inferior -type A and type C-, superior -type B and type D-)). Reduced number of 2D slices (21) were scanned for session 2 and session 3. For all session, scans were repeated with pump on and off to evaluate effects of background phase error. Figure 1 and Figure 2 shows a schema of the acquisition details for all the sessions.
Analysis: 2D PC and 4DFlow net flow measurements were evaluated using Arterys (San Francisco, USA). Background phase correction (BPC) using image-based correction was applied and static phantom correction (pump OFF) was checked to compare the image-based correction. Net flow measurements were considered accurate for a difference less than 5%4 with respect to the ground-truth value measured by the flow meter. Reproducibility was assessed using ICC from session 1 data.
Results
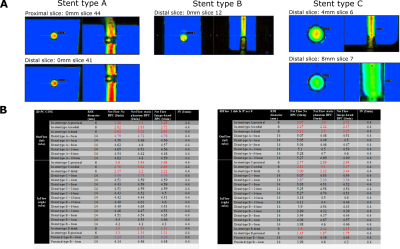
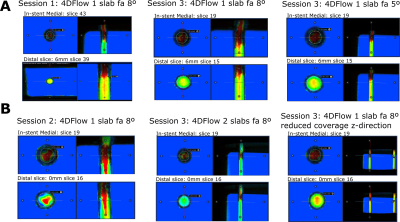
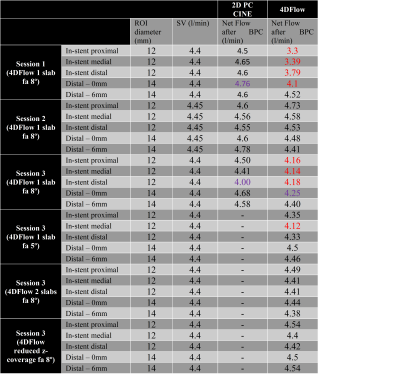
Before placing the stents in session 1 and after placing the stents in areas distal or proximal to the stents, net flow measurements were found accurate after BPC for both 2D and 4DFlow and the reproducibility of repeated measurements was excellent (ICC~1). In-stent measurements were underestimated up to 65% for both 2D and 4DFlow for stents type A, B and C. 2D and 4DFlow net flow measurements for stent A, B and C for session 1 before and after BPC are summarized in Figure 3.Stent type D (platinum-iridium) investigation: More interestingly, net flow measurements from the 2D in-stent slices were found accurate across the 3 sessions. In session 1, the in-stent net flow measurements by 4DFlow showed 7-22% underestimation. We hypothesized that the underestimation could be attributed to the fluid spin history as the stent type D was placed at the exit of the out-flow tube. The 2D vs 4D net flow measurements discrepancy motivated the additional scan sessions investigations. In session 2 with inverted flow direction, stent type D was the first stent of the in-flow tube and we obtained accurate in-stent net flow measurements. For session 3, our findings showed, again, underestimated in-stent net flow measurements for 1 slab whole-volume 4DFlow with flip angle of 8º (5-12% underestimation) and for some in-stent slices for flip angle of 5º (5-7% underestimation) and accurate in-stent net flow measurements for the 2 slab 4DFlow acquisition and the inferior reduced number of slices 1 slab 4DFlow acquisition. Exemplary in-stent and next to stent exemplary ROIs for each 4DFlow acquisition for all session for stent type D are shown in Figure 4. 2D and 4DFlow net flow measurements for stent type D are summarized in Figure 5.
Discussion
This work shows that platinum-iridium stents allow accurate in-stent net flow measurements for both 2D and 4D Flow. Our results also suggest that SNR/VNR and spin history after high susceptibility stents (e.g. stainless steel) may affect the net flow measurements in distal areas after the stent, which can compromise accuracy of downstream flow measurements using 4DFlow with large volume coverage.Acknowledgements
Thanks to Sebastian Endt for helping our during session 3 scanning.References
[1] Avitabile et al., American Journal of Cardiology 2018
[2] Solana et al., ISMRM 2017
[3] Callaghan et al., JMRI 2016
[4] Gatehouse et al, JCMR 2010,
Figures