2104
Impact on Cerebral Perfusion by Black Blood Vessel Wall Imaging Combining with 3D-ASL: Plaque Vulnerability vs. Intracranial Stenosis
Shaoyang Lei1, Chunhui Shan1, Jie Wu1, Jing Wu1, Yunfeng Bao1, Yingmin Chen1, and Shuqian Zhang1
1Hebei General Hospital, Shijiazhuang, China
1Hebei General Hospital, Shijiazhuang, China
Synopsis
Black Blood Vessel Wall Imaging, a valuable tool to detect abnormalities of intracranial vessel walls, was combined with 3D-ASL, a noninvasive approach for detecting cerebral perfusion, to explore the effects of plaque vulnerability and intracranial stenosis on cerebral perfusion. Absolute and relative values of CBF were determined in regions drawn manually based on the territory of blood supply in ASL images. Multivariate regression analysis indicated plaque vulnerability had no significant impact on perfusion while different degrees of luminal narrowing had statistically differences, signifying intracranial stenosis might be a more critical factor for decreased perfusion.
Introduction
Atherosclerosis is a major cause of ischemic stroke. Recently, Black Blood Vessel Wall Imaging (BB-VWI) has emerged as an effective tool to detect abnormalities of extracranial carotid and intracranial vessel walls. Previous studies have shown that abnormal plaque enhancement is a marker of vulnerable plaque after administration of gadolinium contrast agent.1, 2It is well established that plaque vulnerability has higher predictive value for cerebrovascular events than carotid stenosis.3 However, intracranial artery is anatomically distinct from extracranial carotid artery, such as having smaller vascular diameter and more branches, and lacking of intracranial vasa vasorum. It is unproven whether the pattern mentioned above could be the same with intracranial arteries. Here we sought to determine the effects of plaque vulnerability and intracranial stenosis on cerebral blood perfusion by combining BB-VWI and 3D-ASL.Methods
We conducted a retrospective study including 50 intracranial atherosclerotic plaques (V4, 17; PCA, 5; PCOM, 1; ACA, 1; MCA, 19; ICA, 7) from 38 patients (26 men and 12 women; mean age, 55.6 years) who underwent BB-VWI (3D-CUBE, TR, 1300ms; TE, 16.5ms; FOV, 180×180; matrix, 320×320) and 3D-ASL (TR, 4640ms; TE, 10.7ms; TI, 1525ms; FOV, 240×240; matrix, 320×8) between September 2018 and September 2019. Participants were not included if they had plaques on bilateral intracranial arteries or infraction that not caused by intracranial plaque. The dataset from 3D black blood series were used to evaluate abnormalities of intracranial vessels, including vulnerability of plaque and degree of luminal narrowing. Intraplaque hemorrhage (IPH) or abnormal plaque enhancement on contrast-enhanced BB-VWI was defined as vulnerable plaque. Luminal narrowing were classified into three degrees based on NASCET criteria, including mild (10-29%), moderate (30%-69%) and severe stenosis (70-99%). Based on the territory of blood supply, we set up 10 regions of interest (V4/PICA, 1; PCA/PCOM, 3; ACA, 1; MCA/ICA, 5) per hemisphere on axial slices. The regions were chosen on cortical gray matter of territories, including cerebellar hemispheres, pons, midbrain, thalamus, occipital lobe, parietal lobe, temporal lobe, frontal lobe and basal ganglia. For quantitative analysis, bilateral cerebral blood flow (CBF) values of ROIs were obtained in blind method in accordance with plaque carrying artery on 3D-ASL overlaid with DWI. Relative CBF (rCBF) was obtained by normalizing CBF to a region of interest in the contralateral cortical gray matter. Statistic assessments were performed using Chi-square test, One-way ANOVA with Bonferroni, Student’s T test, and multivariate regression analysis. A P value <0.05 was considered to indicate statistical significance.Results and Discussion
Quantitative data from 159 regions with good image quality were analyzed statistically (V4, 17; PCA, 15; PCOM, 3; ACA, 1; MCA, 90; ICA, 33). Mean absolute values of CBF in plaque related territory and contralateral territory were 46.733 and 50.344, respectively (P<0.001), indicating the presence of intracranial plaque was responsible for decreased cerebral blood perfusion. Vulnerable plaque related territory (n=111) had a lower mean rCBF than stable plaque related territory (n=48) (0.911±0.166vs.0.968±0.129, P=0.0177). Mean rCBF in territory associated with mild, moderate and severe stenosis were 0.995, 0.935 and 0.890, respectively (F=6.21, P=0.0025). And there were statistically differences between mild and severe stenosis (P<0.05), indicating severe stenosis had a higher risk of hypoperfusion than mild stenosis. We also performed a multivariate regression analysis to adjust for potential confounders. Multivariate regression analysis demonstrated that rCBF of territory related to moderate and severe stenosis were both 0.13 lower in average than that of mild stenosis (P=0.009, P=0.008), whereas plaque vulnerability had no significant effect on rCBF (P=0.161). In addition, we found that there were 63.0% (70/111) severe stenosis related territories caused by vulnerable plaques while 10.4% (5/48) caused by stable plaques, indicating vulnerable plaque had a higher risk of severe stenosis. The anatomical characteristics of intracranial arteries might determine that intracranial stenosis was a more crucial factor leading to perfusion decreasing than plaque vulnerability. However, given a high risk of rupture, vulnerable plaque detected on BB-VWI also need close attention and timely intervention to prevent acute cerebrovascular events. We were not able to analyze vascular positive remodeling, a minor criteria of vulnerable plaque, given few remodeling segments detected in the present study. Further studies were suggested to take it into consideration for avoiding overestimation of intracranial stenosis.Conclusion
Compared with plaque vulnerability, intracranial stenosis caused by plaques may be a more critical factor in triggering reduction of cerebral blood perfusion.Acknowledgements
No acknowledgement found.References
- Shu JE, Ying ML, Chen XR, et al. Prognostic value of high-resolution magnetic resonance imaging in evaluating carotid atherosclerotic plaque in patients with ischemic stroke. Medicine (Baltimore). 2017;96(45):e8515.
- Natori T, Sasaki M, Miyoshi M, et al. Intracranial Plaque Characterization in Patients with Acute Ischemic Stroke Using Pre- and Post-Contrast Three-Dimensional Magnetic Resonance Vessel Wall Imaging. J Stroke Cerebrovasc Dis. 2016;25(6):1425-1430.
- Qiao Y, Zeiler SR, Mirbagheri S, et al. Intracranial plaque enhancement in patients with cerebrovascular events on high-spatial-resolution MR images. Radiology. 2014;271(2):534-542.
Figures
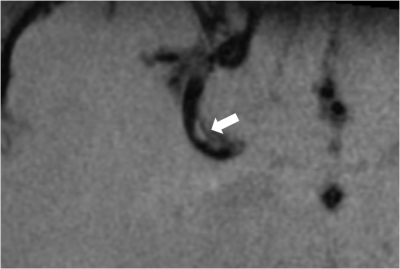
CUBE. A 43-y-old man had an atherosclerotic
plaque of the right middle cerebral artery with eccentric
hyperintensity on anterior wall, consistent with intraplaque hemorrhage (IPH).
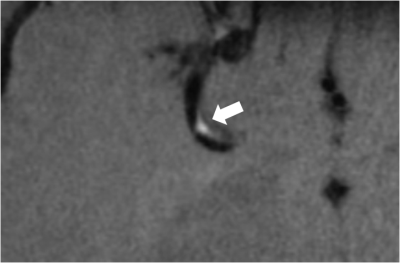
CE-CUBE. The right MCA plaque with severe
luminal stenosis still showed eccentric hyperintensity after contrast
enhancement.

TOF-MRA. A severe stenosis of right MCA was
displayed on white blood image, with few distal branches detected.
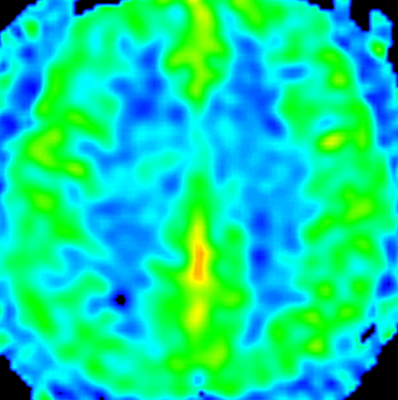
3D-ASL(PLD=1.5s). There were no significant
differences of CBF between bilateral frontoparietal cortexes, which were supplied by MCA.