2101
Assessment of myocardial fractional blood volume using Fe-MRI and 3-compartment model of capillary level water exchange in patients with CKD
Douglas Black1, Sokratis Stoumpos1, Michael Jerosch-Herold2, Neil Chatterjee3, Peter Gatehouse4, Geeshath Jayasekera1, Timothy Carroll5, David Kingsmore1, Colin Berry1, Patrick Mark1, Giles Roditi1, and Aleksandra Radjenovic1
1University of Glasgow, Glasgow, United Kingdom, 2Harvard Medical School, Boston, MA, United States, 3University of Pennsylvania, Philadelphia, PA, United States, 4Imperial College, London, United Kingdom, 5University of Chicago, Chicago, IL, United States
1University of Glasgow, Glasgow, United Kingdom, 2Harvard Medical School, Boston, MA, United States, 3University of Pennsylvania, Philadelphia, PA, United States, 4Imperial College, London, United Kingdom, 5University of Chicago, Chicago, IL, United States
Synopsis
Estimates of myocardial fractional blood volume (FBV), capillary level vascular-interstitial water exchange rate and permeability surface area product were obtained in a cohort of chronic kidney disease (CKD) patients and a control set of healthy volunteers using iron-enhanced MRI (Fe-MRI). FBV was elevated in females, in both CKD patients and control subjects. Fe-MRI also demonstrated reduced permeability surface area product in CKD patients compared to healthy controls, and may provide unique insights into microvascular pathophysiology, particularly in patients with contraindications to gadolinium-based contrast agents.
Background
Patients diagnosed with chronic kidney disease (CKD) are not able to benefit from diagnostic imaging involving gadolinium based contrast agents (GBCA). Intravascular iron-based contrast agent ferumoxytol provides a potential alternative to GBCA for the diagnosis of cardiovascular pathologies in CKD. The benefits of ferumoxytol-enhanced magnetic resonance angiography (MRA) are already well established. However, the potential utility of ferumoxytol in the assessment of myocardial microvasculature is still insufficiently explored. We have obtained estimates of myocardial fractional blood volume (FBV) and vascular-interstitial water exchange rate in a cohort of CKD patients and a control set of healthy volunteers using iron-enhanced MRI (Fe-MRI).Methods
Twenty six patients with severe CKD and eleven healthy volunteers (HV) were recruited following approval by two regional ethics boards (CKD - 18 male; median age 58 (29 - 76); BW = 75 ± 18 kg; BMI = 27 ± 6 kg/m2; HV – 6 male, median age 30 (22 - 61); BW 88 ± 19 kg; BMI = 28 ± 5 kg/m2). CKD subjects were scanned on a 3T Prisma and healthy volunteers on a 1.5T Aera (Siemens Healthcare).All subjects received fractionated injections of diluted ferumoxytol (1:5), up to the maximal dose of 3mg/kg. T1 maps of the mid-ventricular left myocardium were acquired using a modified Look Locker inversion recovery method (MOLLI) before contrast and following each fractionated injection. Paired R1myo and R1blood values (1/T1 [s-1]) were recorded at each step.
Three-compartment 2-exchange sites model [1] was used to estimate fractional blood volume (FBV, unit free fraction), vascular-interstitial exchange rate (kvi [s-1]) and their product FBV* kvi (proportional to permeability surface area product (PS, [s-1])). Model assumptions included a fixed extracellular volume (ECV) of 0.3 for CKD patients and a lower value of 0.25 for controls. Intracellular water lifetime of 100 ms was assumed in all subjects. Non-parametric Mann Whitney and Kruskal-Wallis tests were used to assess the differences in model parameters.
Results
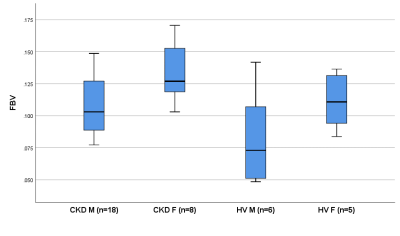
In CKD subjects, FBV estimated using a 3-compartment model was 0.12 ± 0.03 compared to 0.10 ± 0.03 in healthy volunteers (p = 0.115). The distribution of estimated vascular-interstitial exchange rates kvi was 4.6 ± 2.0 s-1 vs 12.2 ± 10.9 s-1, (p = 0.07). PS (0.51 ± 0.20 s-1 vs 0.88 ± 0.55 s-1) varied between CKD and HV subgroups (Mann Whitney p = 0.047).There were significant differences in FBV between males and females: 0.10 ± 0.03 vs 0.13 ± 0.02, p = 0.015.
Distribution of FBV in four subject subgroups: CKD Male (n = 18), CKD Female (n = 8), HV Male (n = 6) and HV female (n = 5) is illustrated in Figure 1. There were significant differences in FBV (Kruskall-Wallis test for differences between four subgroups: p = 0.022). There were no gender differences in other model parameters.
Discussion
Our results suggest that patients suffering from chronic kidney disease appear to have lower permeability surface area product than well matched healthy controls. FBV values showed no statistically significant differences between the CKD and control group, although we observed pronounced gender differences that are present both in health and disease (Figure 1).CKD patients seem to have largely preserved (if not elevated) resting myocardial fractional blood volume compared to sex-matched controls. The differences in water exchange rates between the interstitial and vascular compartment and permeability surface area product point to the possible alterations in the architecture and function of capillaries supplying the myocardial tissue in patients with CKD. Given that FBV is expected to correlate with microvascular surface area, reduced values of PS with preserved (or elevated) FBV suggest the reduction in blood vessel permeability.
Conclusion
Although our sample size is small, and two sets of data were acquired using slightly different acquisition protocols, the results presented here strongly suggest that Fe-MRI has the potential to provide a unique insight into the nature of microvascular pathology in chronic kidney disease and other diseases affecting myocardium.Of particular interest is our finding that gender differences in myocardial FBV exist both in healthy volunteers and patients with CKD, with possible implications on mechanisms of drug delivery and monitoring effects of therapies.