2100
Pressure-volume Relationship by Stress Cardiovascular Magnetic Resonance: feasibility and clinical implications1MRI Unit, Fondazione G. Monasterio CNR-Regione Toscana, Pisa, Italy, 2University of Trieste, Trieste, Italy, 3University of Palermo, Palermo, Italy, 4Università Campus Bio-Medico, Roma, Italy
Synopsis
We showed for the first time that the ΔESPVR index, an index of myocardial contractile function easily obtained during routine stress echocardiography, can be noninvasively calculated during a dipyridamole stress-CMR exam. The ΔESPVR index was independent from baseline LV dimensions and function while it was lower in patients with myocardial fibrosis and in patients with abnormal stress CMR. At receiver-operating characteristic curve analysis, a ΔESPVR<0.02 predicted the presence of future cardiac events, being useful for additional prognostic stratification.
Introduction
The variation between rest and peak stress end-systolic pressure-volume relation (ESPVR; the Suga index) is easily obtained during routine stress echocardiography and has been established as a reasonably load-independent index of myocardial contractile performance that provides prognostic information above and beyond regional wall motion.1,2This is the first study assessing the delta rest-stress ESPVR (ΔESPVR) by stress Cardiovascular Magnetic Resonance (CMR).
Methods
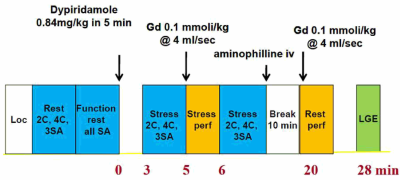
One-hundred consecutive patients (24 females, mean age 63.76±10.17 years) who underwent dipyridamole stress-CMR (Figure 1) in a high volume CMR Laboratory were considered.Systolic blood pressures at rest and stress were recorded in the right arm by using a MR‐compatible sphygmomanometer. The end-systolic pressure was obtained as LV end-systolic pressure=0.9*systolic blood pressure. Left ventricular (LV) end-diastolic and end-systolic volumes (EDV, ESV) were obtained at rest and at peak of stress from apical vertical long-axis view and horizontal long-axis view using the biplane Simpson’s method. The ESPVR (mmHg/mL/m2) was obtained as the ratio of the end-systolic pressure to the LVESVI. The ESPVR was determined at rest and at peak stress. The ΔESPVR was calculated as the variation between rest and peak stress ESPVR.2,3
Abnormal wall motion and perfusion at rest and after dipyridamole were analysed.
Macroscopic myocardial fibrosis was detected by the late gadolinium enhancement (LGE) technique.
Results
Mean ESPVR index at rest and peak stress was, respectively, 4.84±2.47 mmHg/mL/m2 and 5.33±3.16 mmHg/mL/m2 and mean ΔESPVR index was 0.48±1.45 mmHg/mL/m2.ΔESPVR index was significantly lower in males than in females. ΔESPVR index was not correlated to baseline left ventricular end-diastolic volume index or ejection fraction.
Forty-three patients had myocardial fibrosis detected by the LGE technique and they showed significantly lower ΔESPVR values (Figure 2A).
An abnormal stress CMR was found in 25 patients (19 reversible stress perfusion defect in at least one myocardial segment and 6 reversible stress perfusion defect plus worsening of stress wall motion in comparison with rest). The ΔESPVR index was significantly lower in patients with abnormal stress CMR (Figure 2B).
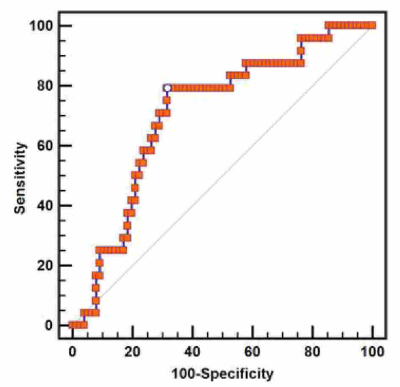
During a mean follow-up of 56.34±30.04 months, 24 cardiovascular events occurred. At receiver-operating characteristic curve analysis, a ΔESPVR<0.02 predicted the presence of future cardiac events with a sensitivity of 0.79 and a specificity of 0.68 (Figure 3).
Conclusions
We showed for the first time that the noninvasive assessment of the ΔESPVR index during a dipyridamole stress-CMR exam was feasible. The ΔESPVR index was independent from baseline LV dimensions and function and, as a consequence, can be used for a comparative assessment of patients with different diseases. ΔESPVR by CMR can be a useful and simple marker for additional prognostic stratification.Acknowledgements
No acknowledgement found.References
1. Grosu A, Bombardini T, Senni M, Duino V, Gori M, Picano E. End-systolic pressure/volume relationship during dobutamine stress echo: a prognostically useful non-invasive index of left ventricular contractility. Eur Heart J 2005;26(22):2404-2412.
2. Bombardini T, Zoppe M, Ciampi Q, et al. Myocardial contractility in the stress echo lab: from pathophysiological toy to clinical tool. Cardiovasc Ultrasound 2013;11:41.
3. Bombardini T, Mulieri LA, Salvadori S, et al. Pressure-volume Relationship in the Stress-echocardiography Laboratory: Does (Left Ventricular End-diastolic) Size Matter? Rev Esp Cardiol (Engl Ed) 2017;70(2):96-104.