2099
The additive prognostic value of end-systolic pressure-volume relation by stress CMR in patients with known or suspected coronary artery disease1MRI Unit, Fondazione G. Monasterio CNR-Regione Toscana, Pisa, Italy, 2University of Trieste, Trieste, Italy, 3University of Palermo, Palermo, Italy, 4Università Campus Bio-Medico, Roma, Italy
Synopsis
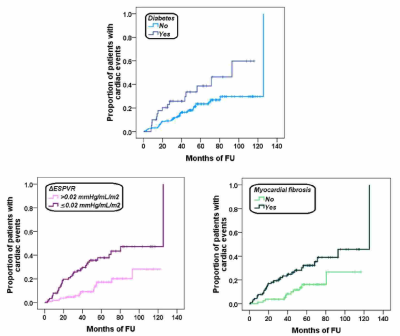
We assessed for the first time the prognostic value of the ΔESPVR (difference between peak and rest end-systolic pressure-volume relation) index evaluated during dipyridamole stress-CMR in 196 patients with known or suspected coronary artery disease. During a mean follow-up time of 53.17±28.21 months 50 cardiac events were recorded. In the multivariate analysis the independent predictive factors for cardiac events were diabetes, a ΔESPVR index≤0.02 mmHg/mL/m2, and myocardial fibrosis.
Introduction
The variation between rest and peak stress end-systolic pressure-volume relation is an afterload-independent index of left ventricular contractility.1 This index is easily obtained during routine stress echocardiography1,2 but can be derived also during a stress cardiovascular magnetic resonance (CMR) exam, that is the gold standard for the quantification of biventricular volumes.3The aim of this study was to assess for the first time the prognostic value of delta rest-stress ESPVR (ΔESPVR) by dipyridamole stress-CMR in patients with known or suspected coronary artery disease (CAD).
Methods
One-hundred and ninety-six consecutive patients (49 females, mean age 62.74±10.66 years) who underwent dipyridamole stress-CMR in a high volume CMR Laboratory were considered.Abnormal wall motion and perfusion at rest and after dipyridamole were analysed.
Macroscopic myocardial fibrosis was detected by the late gadolinium enhancement (LGE) technique.
Systolic blood pressures at rest and stress were recorded in the right arm by using a MR‐compatible sphygmomanometer. The end-systolic pressure was obtained as LV end-systolic pressure=0.9*systolic blood pressure. Left ventricular (LV) end-diastolic and end-systolic volumes (EDV, ESV) were obtained at rest and at peak of stress from apical vertical long-axis view and horizontal long-axis view using the biplane Simpson’s method. The ESPVR (mmHg/mL/m2) was obtained as the ratio of the end-systolic pressure to the LVESVI. The ESPVR was determined at rest and at peak stress. The ΔESPVR was calculated as the variation between rest and peak stress ESPVR.1,4
Results
An abnormal stress CMR was found in 52 (26.5%) patients; 36 patients had a reversible stress perfusion defect in at least one myocardial segment and 16 a reversible stress perfusion defect plus worsening of stress wall motion in comparison with rest.LGE sequences were acquired in 170 (86.7%) patients and myocardial fibrosis was detected in 90 patients (52.9%).
A ΔESPVR index≤0.02 mmHg/mL/m2 was found in 88 patients (44.9%).
Mean follow-up time was 53.17±28.21 months (median=49.61 months). Cardiac events were recorded in 50 (25.5%) patients: 5 cardiac deaths, 17 revascularizations for angina (N=14) or myocardial infarction (N=3), one myocardial infarction, 23 hospitalisations for heart failure (N=5) or unstable angina (n=18), and 4 ventricular arrhythmias. Table 1 shows the results of the univariate Cox analysis. Diabetes, family history, LVEF, abnormal stress CMR, myocardial fibrosis, and reduced ΔESPVR were significant univariate prognosticators. In the multivariate analysis the independent predictive factors were diabetes (HR=2.33, 95%CI=1.21-4.51, P=0.012), a ΔESPVR index≤0.02 mmHg/mL/m2 (HR=2.58, 95%CI=1.29-5.13, P=0.007), and myocardial fibrosis (HR=2.13, 95%CI=1.05-4.31, P=0.036). The Kaplan Meyer curves showing the impact of each prognostic factor on the development of cardiac events are shown in Figure 1. The log-rank test revealed a significant difference in all the curves (diabetes: P=0.016, ΔESPVR index≤0.02 mmHg/mL/m2: P<0.0001, and myocardial fibrosis: P=<0.0001).
Conclusions
ΔESPRV assessed by CMR provides a prognostic stratification in patients with known or suspected coronary artery disease, in addition to that supplied by diabetes and myocardial fibrosis.Acknowledgements
No acknowledgement found.References
1. Bombardini T, Mulieri LA, Salvadori S, et al. Pressure-volume Relationship in the Stress-echocardiography Laboratory: Does (Left Ventricular End-diastolic) Size Matter? Rev Esp Cardiol (Engl Ed) 2017;70(2):96-104.
2. Grosu A, Bombardini T, Senni M, Duino V, Gori M, Picano E. End-systolic pressure/volume relationship during dobutamine stress echo: a prognostically useful non-invasive index of left ventricular contractility. Eur Heart J 2005;26(22):2404-2412.
3. Hundley WG, Bluemke DA, Finn JP, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation 2010;121(22):2462-2508.
4. Bombardini T, Zoppe M, Ciampi Q, et al. Myocardial contractility in the stress echo lab: from pathophysiological toy to clinical tool. Cardiovasc Ultrasound 2013;11:41.