2049
Influence of hydration status on myocardial T1 and T2 relaxation time measurements: an intraindividual study in healthy volunteers1Radiology, Universityhospital Bonn, Bonn, Germany
Synopsis
Myocardial T1 and T2 mapping allow for non-invasive quantification of myocardial tissue alterations. Several confounders can influence correct relaxation time assessment. However, the effect of physiological changes in myocardial water content has not been investigated yet. In an intraindividual cardiac magnetic resonance imaging (MRI) study, we investigated 12 healthy volunteers at baseline, after 10-12 hours of fasting and after rehydration. Especially after dehydration, T1 and T2 relaxation times were reduced compared to baseline indicating a detectable effect of the hydration status on relaxation time assessment. Hydration status should therefore be recognized as a possible confounder of T1 and T2 mapping.
Introduction
Myocardial T1 and T2 mapping allow for a non-invasive quantification of myocardial tissue alterations across a broad range of myocardial disease in patients eligible for cardiac magnetic resonance imaging (MRI) 1. As myocardial mapping of is very sensitive for the detection of myocardial tissue abnormalities like myocardial edema or fibrosis, current guidelines (e.g. for inflammatory cardiomyopathies) already recommend the implementation of mapping techniques into clinical routine 2. However, it is important to know that mapping techniques can be prone to confounders such as heart rate and magnetic field inhomogeneities 1. Apart from these variations caused by confounders, there are also subtle differences in myocardial T1 and T2 relaxation times that are related to gender, age or myocardial iron content, which might alter correct assessment of myocardial relaxation times 1. Although it is well known that myocardial T1 and T2 relaxation are sensitive to pathological increase of myocardial water content (e.g. myocardial edema), 3 the influence of physiological hydration changes as a possible confounder of relaxation time assessment has not been fully evaluated yet. Although previous experimental studies suggest that alterations in MRI relaxation times occur with nonpathological alterations in myocardial water content, 4 no actual in vivo data is available on the relationship between changes in myocardial water content and concordant myocardial T1 and T2 relaxation time measurements. Thus, the purpose of this study was to evaluate whether the change in myocardial water content due to dehydration and hydration might alter the correct assessment of myocardial relaxation times in healthy volunteers.Methods
The institutional review board approved this prospective study and all subjects gave written informed consent. The study population consisted of healthy volunteers without known previous cardiovascular disease and without cardiac risk factors. All cardiac MRI scans were performed on a 1.5 Tesla whole body system. Three CMR scans were performed in each study participants: The baseline scan (normal scan) was performed during the morning hours. After 12 hours of fasting (no access to food or water) another scan was performed (dehydration scan). The last scan was performed after adequate hydration and drinking of 1.5 liter immediately before the investigation (hydration scan). Cardiac MRI scans allowed for assessment of cardiac function, and the assessment of myocardial T1 and T2 relaxation times. For functional analysis ECG-gated steady-state free precession cine images were obtained. For myocardial T1 mapping, a modified Look-Locker inversion recovery (MOLLI) acquisition scheme was used. For myocardial T2 mapping, a six-echo gradient spin-echo sequence was applied. Parametric maps were acquired in basal, midventricular, and apical sections and global T1 and T2 relaxation times were calculated. Blood pressure measurements and laboratory markers were obtained prior to every cardiac MRI scan. For multiple comparisons, the Friedman test followed by Dunn’s multiple comparisons test was used.Results
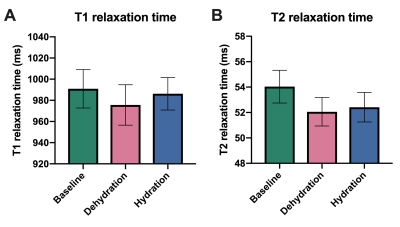
12 healthy volunteers (5 men, 7 women, mean age: 25.8 ± 3.2 years) were investigated in this study. There was no change in systolic blood pressure (124.1 ± 11.61 mmHg (baseline) vs. 121.3 ± 10.37 mmHg (dehydration) vs. 121.0 ± 10.1 mmHg (hydration); P=0.282) or left ventricular ejection fraction (64.8 ± 3.8 % (baseline) vs. 62.3 ± 3.7 % (dehydration) vs. 66.9 ± 4.5 % (hydration); P=0.179) between the different MRI scans. T1 relaxation times were slightly, but significantly reduced in dehydration (990.9±28.6 ms (baseline) vs. 975.7±30.1 ms (dehydration) vs. 986.2±24.1 ms (hydration); P=0.009). Similar results were observed for T2 relaxation times (54.04±2.03 ms (baseline) vs. 52.06±1.76 ms (dehydration) vs. 52.41±1.83 ms (hydration); P=0.005) (see Figure 1).Discussion
Our results indicate that in healthy volunteers, hydration status influences myocardial T1 and T2 relaxation times. Particularly in a dehydrated state, significant alterations in relaxation times compared to baseline measurements were observed. During dehydration myocardial relaxations times were reduced compared to baseline. Water loss due to water deprivation or inadequate water intake typically leads to hypertonic dehydration. In hypertonic dehydration water loss exceeds sodium loss, which is characterized by an osmotic shift of water from the intracellular to the extracellular compartment. The relatively lower amount of water in the intracellular compartment might influence T1 and T2 relaxation times measurements. Although differences in myocardial T1 after dehydration compared to baseline were rather small (15.2±18.8 ms), hydration status might be an additional confounder the clinician should have in mind when interpretating results, especially in follow-up studies and in cases of subtle myocardial disease or fibrosis.Conclusions
Hydration status might influence myocardial T1 and T2 relaxation times. Particularly, dehydration may lead to significant alterations in relaxation times and thereby may influence correct assessment of T1 and T2 relaxation times. Hydration status should be recognized as new potential confounder of correct T1 and T2 relaxation time assessment in clinical routine. Future studies should assess the influence of dehydration and hyperhydration on MRI relaxation time measurements in a clinical setting.Acknowledgements
None.References
1. Messroghli DR, Moon JC, Ferreira VM, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: A consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson. 2017;19:75.
2. Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J Am Coll Cardiol. 2018;72:3158-3176.
3. Luetkens JA, Faron A, Isaak A, et al. Comparison of Original and 2018 Lake Louise Criteria for Diagnosis of Acute Myocarditis: Results of a Validation Cohort. Radiol Cardiothorac Imaging. 2019;1:e190010.
4. Brown JJ, Andre MP, Slutsky RA. Proton nuclear magnetic resonance tissue analysis of normal, volume overloaded, and dehydrated rabbit myocardium. Am Heart J 1984;108:159-64.